Baby news is everywhere—celebrity bump speculation, plot twists in streaming dramas, and friends posting “we’re trying” updates like it’s a season finale.

At the same time, real-world headlines about reproductive policy and court decisions remind people that family-building is both personal and public.
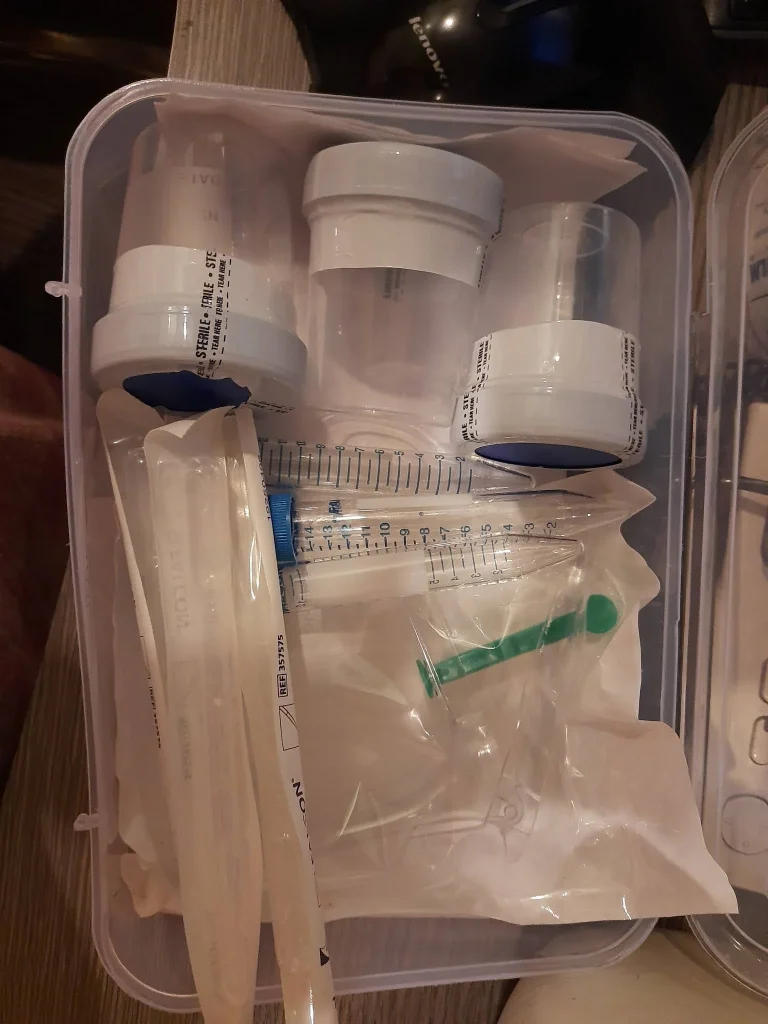
If you’re considering ICI at home, a home insemination kit can support a lower-intervention path—when you pair it with clean technique, thoughtful screening, and clear consent.
Is at-home insemination (ICI) a realistic alternative to IVF right now?
For some people, yes. ICI (intracervical insemination) is often discussed as a home fertility option when you want to start with something simpler than clinic-based treatment.
It’s not a replacement for IVF in every situation. IVF can be the right next step when there are known fertility factors, when timing attempts haven’t worked, or when a clinician recommends it. Still, many LGBTQ+ families, solo parents by choice, and couples navigating costs start by exploring ICI because it can feel more accessible and more private.
What ICI does (and doesn’t) do
ICI places sperm near the cervix. It doesn’t bypass the cervix the way IUI does in a clinic, and it doesn’t involve eggs or embryos like IVF. Thinking of it as “a supportive method for timing and placement” keeps expectations grounded.
What safety steps matter most when using a home insemination kit?
In the middle of all the internet chatter, the basics are still the basics: cleanliness, single-use supplies, and avoiding anything that raises infection risk. A home insemination kit is designed to help with controlled placement, but technique and hygiene do the heavy lifting.
Clean setup checklist (plain-language)
- Wash hands thoroughly and prep a clean surface.
- Use sterile, single-use items (syringes, containers) and keep packaging closed until you need it.
- Avoid non-sterile additives (saliva, household oils). If lubricant is used, choose one that’s fertility-friendly and used sparingly.
- Don’t reuse tools even if they “look clean.”
If anything causes sharp pain, fever, unusual discharge, or symptoms that worry you, seek medical care. Safety always outranks sticking to a plan.
How should we think about screening and sperm handling?
People often focus on timing and forget that screening choices are part of risk reduction too. That’s especially true when using a known donor. Bank donor pathways typically include standardized testing and quarantine processes, while known-donor arrangements can vary widely.
If you’re deciding between options, map it like a production schedule: who provides what, when testing happens, how results are shared, and how consent is documented. This approach can reduce stress later.
Known donor: what to clarify early
- Testing expectations and frequency
- Abstinence windows and collection logistics
- Communication boundaries (before, during, after attempts)
- Parenting intentions and legal steps
Do legal headlines affect at-home insemination choices?
They can. Recent coverage has highlighted how reproductive health and rights are being debated in courts and through policy, and how those decisions can ripple into family-building. Separately, news about a Florida court ruling involving at-home artificial insemination has many people re-checking assumptions about donor intent and parental rights.
Because laws differ by state and country, the safest move is to treat legal clarity as part of the plan, not an afterthought. If you’re using a known donor, consider getting legal advice in your area and documenting consent and intentions in writing.
For a general overview tied to the headlines, see this Florida Supreme Court makes ruling in at-home artificial insemination case.
Is the “fertility cliff at 35” real, or just loud online?
The number shows up everywhere—think political talking points, lifestyle podcasts, and the kind of celebrity pregnancy discourse that fuels comment sections. But the more useful takeaway is calmer: fertility changes over time, and it’s influenced by multiple factors for people with ovaries and people with testes.
If age is on your mind, focus on what you can control this cycle: tracking ovulation, planning attempts, and choosing the least risky method that fits your situation. If you’re unsure where you stand, a clinician can help interpret labs and history without jumping straight to IVF.
What should we document so we feel confident later?
Documentation isn’t just for worst-case scenarios. It can also reduce misunderstandings and protect relationships. A simple folder—digital or paper—can be a relief when emotions run high.
- Donor agreements or intent letters (especially with a known donor)
- Testing dates/results (as shared and agreed)
- Cycle notes (ovulation tests, timing, symptoms)
- Receipts/lot numbers for supplies, if relevant
Which supplies help ICI feel simpler at home?
The goal is a setup that’s straightforward, clean, and not improvised. If you’re searching for an option built for this purpose, consider an at-home insemination kit for ICI that’s designed to support controlled placement and a less stressful routine.
How does at-home insemination (ICI) work?
Medical disclaimer
This article is for general education and does not provide medical or legal advice. It can’t diagnose fertility conditions or replace care from a qualified clinician. If you have pain, bleeding, fever, a history of pelvic infection, or questions about medications, testing, or legal parentage, talk with a licensed healthcare professional and an attorney in your jurisdiction.