On a rainy weeknight, an anonymous couple sat on the edge of their bed with a phone timer, a towel, and a grocery bag of “just in case” supplies. They’d watched a comfort-show episode where the characters face yet another pregnancy obstacle, and it hit a little too close. They weren’t looking for TV drama. They wanted a simple, private way to try.
If that sounds familiar, you’re not alone. At-home insemination (ICI) keeps showing up in real life conversations—next to celebrity pregnancy chatter, streaming-true-crime buzz, and headlines about courts weighing in on donor rights. Below is the no-fluff guide to using a home insemination kit for ICI: timing, comfort, positioning, and clean-up.
Medical disclaimer: This article is educational and not medical advice. It can’t diagnose or treat any condition. If you have pain, heavy bleeding, repeated negative tests after trying, or a known medical concern, talk with a qualified clinician or fertility specialist.
What exactly is ICI at home—and who is it for?
ICI stands for intracervical insemination. It’s a method where sperm is placed near the cervix using a syringe-style applicator. People often consider ICI when they want a lower-intervention option before moving to IUI or IVF, or when clinic access is limited.
ICI can be part of LGBTQ+ family-building, solo parent journeys, and couples dealing with barriers to intercourse. It can also be a practical step when you’re not ready—financially, emotionally, or logistically—for IVF.
ICI vs. IUI vs. IVF in one minute
- ICI: At home, sperm placed at the cervix.
- IUI: In a clinic, washed sperm placed in the uterus.
- IVF: Eggs retrieved, fertilized in a lab, embryo transferred.
When should you try ICI if timing is everything?
Timing is the make-or-break variable people talk about most. It’s also where social media advice gets messy fast. The goal is to inseminate close to ovulation, when cervical mucus is most sperm-friendly and an egg may be released soon.
Practical ways people time ICI
- Ovulation test strips (LH tests): Useful for catching the surge that often happens 24–36 hours before ovulation.
- Cervical mucus changes: Many notice clearer, stretchier mucus in the fertile window.
- Basal body temperature (BBT): Confirms ovulation after it happens, which helps for planning future cycles.
Age headlines don’t help here. You may have seen recent discussions pushing back on the idea that fertility “falls off a cliff” at 35. The more useful takeaway is this: fertility is individual, and your best move is to get cycle-specific data rather than rely on a single scary number.
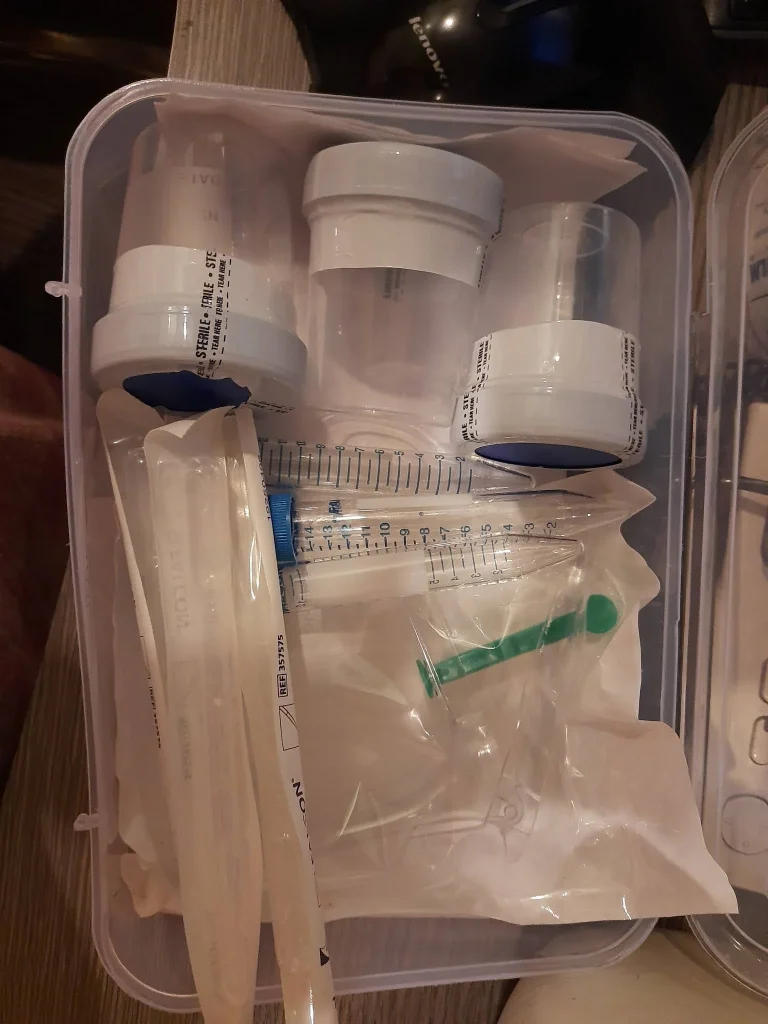
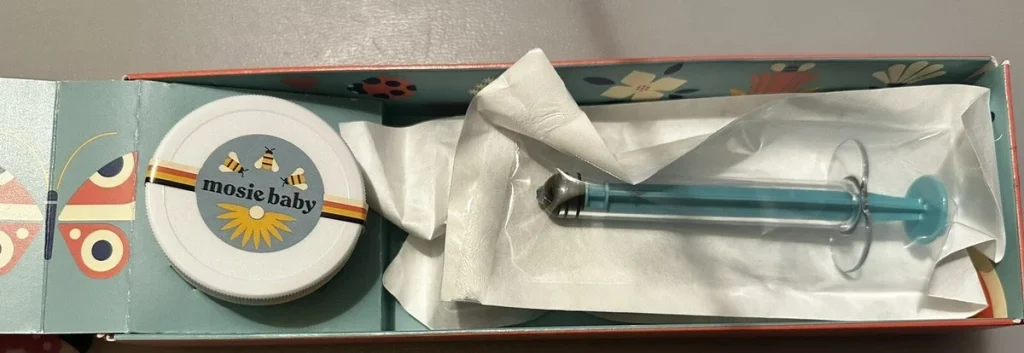
What should be in a home insemination kit (and what should not)?
People sometimes try to DIY with random syringes or household items. That can increase irritation and contamination risk. A purpose-made kit focuses on comfort, safer materials, and ease of use when you’re already nervous.
Basics that support a smoother attempt
- Needle-free syringe designed for insemination
- Collection container if using fresh sperm
- Clear instructions you can follow under stress
- Optional items for comfort and clean-up (pads, towels)
If you’re comparing options, start with a product that’s designed specifically for ICI and includes guidance. Here’s a related option to review: at-home insemination kit for ICI.
How do you make ICI more comfortable (without overcomplicating it)?
Comfort matters because tension can turn a straightforward process into a frustrating one. The goal is a calm routine you can repeat, not a perfect “fertility ritual.”
Set the room, then set expectations
- Choose a time when you won’t be rushed or interrupted.
- Warm the room and gather supplies first to avoid mid-process scrambling.
- Plan for a normal amount of leakage afterward; it’s common and not a sign of failure.
Positioning: what people actually do
Many people lie on their back with knees bent. Some place a pillow under the hips for comfort. There’s no universally proven angle that guarantees success, so pick a position that helps you relax and keep the process steady.
What does the step-by-step ICI flow look like?
Exact instructions can vary by kit and sperm source, so always follow the directions that come with your supplies and any sperm bank guidance. At a high level, most at-home ICI attempts follow this rhythm:
- Prep: Wash hands, set out supplies, start a timer.
- Collect or thaw: Follow source-specific handling rules.
- Load syringe: Avoid bubbles when possible and move slowly.
- Inseminate: Gently place sperm near the cervix.
- Rest: Many choose 10–20 minutes to stay relaxed.
- Clean up: Expect some backflow; use a pad if helpful.
If you feel sharp pain, dizziness, fever, or unusual bleeding, stop and seek medical care.
What about legal and donor issues—why is this suddenly in the news?
Recent reporting has highlighted court decisions involving at-home insemination and whether a sperm donor automatically gives up parental rights. The specifics vary by state and situation, but the cultural takeaway is clear: informal arrangements can create real legal ambiguity.
If you’re using a known donor, consider legal support before trying—especially if you’re counting on clear parental rights from day one. For background reading tied to the recent coverage, see: Florida Supreme Court makes ruling in at-home artificial insemination case.
How do you decide whether to keep trying ICI or move to a clinic?
Think in checkpoints, not pressure. Some people try a few well-timed cycles and then reassess. Others move sooner if they’re using frozen sperm, have irregular cycles, or want diagnostic testing.
Signals to consider extra support
- Cycles are unpredictable and timing feels like guesswork.
- You’ve tried multiple cycles with good timing and no success.
- You want clarity on ovulation, sperm parameters, or underlying conditions.
Common questions you can answer before your next attempt
- Do we have a timing plan (LH tests, symptoms, calendar)?
- Are we using tools made for insemination, not improvised supplies?
- Do we have a clean-up plan so we can rest afterward?
- If using a known donor, do we understand local legal realities?
Pop culture loves an “obstacles” storyline—new seasons, new characters, bigger twists. Your fertility plan doesn’t need that energy. With a clear window, a steady technique, and the right home insemination kit, ICI can be a grounded next step that keeps you in control.