Is at-home insemination actually a realistic option?
Does using a home insemination kit make the process safer or just simpler?
And why does it feel like everyone—from celebrity baby news to courtrooms—is talking about fertility right now?
Yes, at-home insemination (often called ICI, or intracervical insemination) can be a practical path for some people. A home insemination kit can also make the logistics less stressful, especially when you’re trying to stay calm and present. As for the cultural noise: it’s everywhere. Entertainment coverage keeps pregnancy announcements in the spotlight, and legal headlines keep reminding us that family-building isn’t only medical—it can be personal, political, and paperwork-heavy.
This guide walks through the big picture, the feelings that come up, the practical steps, and the safety/testing basics—without assuming what your family looks like. (Hello, solo parents by choice, LGBTQ+ families, known donors, and everyone in between.)
Big picture: Why ICI at home is trending again
When celebrity pregnancy roundups hit your feed, it can make pregnancy look effortless and perfectly timed. Real life is usually messier. Meanwhile, reproductive health litigation and shifting state-by-state rules keep showing up in the news, which can add urgency to planning.
At the same time, more people are rethinking the idea that fertility has a hard cliff at 35. The more accurate takeaway is nuanced: age can matter, but it’s not the only variable. Ovulation patterns, sperm health, underlying conditions, stress, and access to care all shape the story.
That mix—pop culture pressure + legal uncertainty + “what about my timeline?” anxiety—pushes many people to explore lower-intervention options first, including ICI at home as a step before moving to medicated cycles, IUI, or IVF.
Emotional considerations: The part nobody puts in a headline
Trying at home can feel empowering. It can also feel surprisingly intense. The same bedroom that’s meant for rest can start to feel like a “testing site,” especially if each cycle begins to carry more meaning.
Pressure shows up differently for each person
One partner might want structure and data. Another might want romance and spontaneity. Neither is wrong, but unspoken expectations can turn timing into tension.
Conversation starters that lower the temperature
- “What would make this feel emotionally safe for you?”
- “Do you want this to feel intimate, clinical, or somewhere in between?”
- “If this cycle doesn’t work, what kind of support do you want the next day?”
If you’re using donor sperm (known or from a bank), add one more layer: clarity. People often assume they’re aligned until they’re not. It’s kinder to everyone to talk through expectations early.
Practical steps: A clear, low-drama ICI plan
ICI is typically about placing sperm in the vagina near the cervix around the fertile window. It’s not the same as IVF, and it’s also different from IUI (which is done in a clinic and places sperm into the uterus).
1) Decide what “home” means for you
Home can mean your home, a partner’s home, or any private space where you can relax and control the environment. Comfort matters more than perfection.
2) Track the fertile window in a way you can sustain
Some people use ovulation predictor kits. Others track cervical mucus, basal body temperature, or cycle patterns. The best method is the one you’ll actually keep doing without burning out.
3) Plan the handoff (especially with a known donor)
Timing and communication are everything. Decide in advance how you’ll handle delays, privacy, and boundaries. If you need a script, try: “We’re aiming for the fertile window, so we’ll confirm timing the day-of. Thank you for being flexible.”
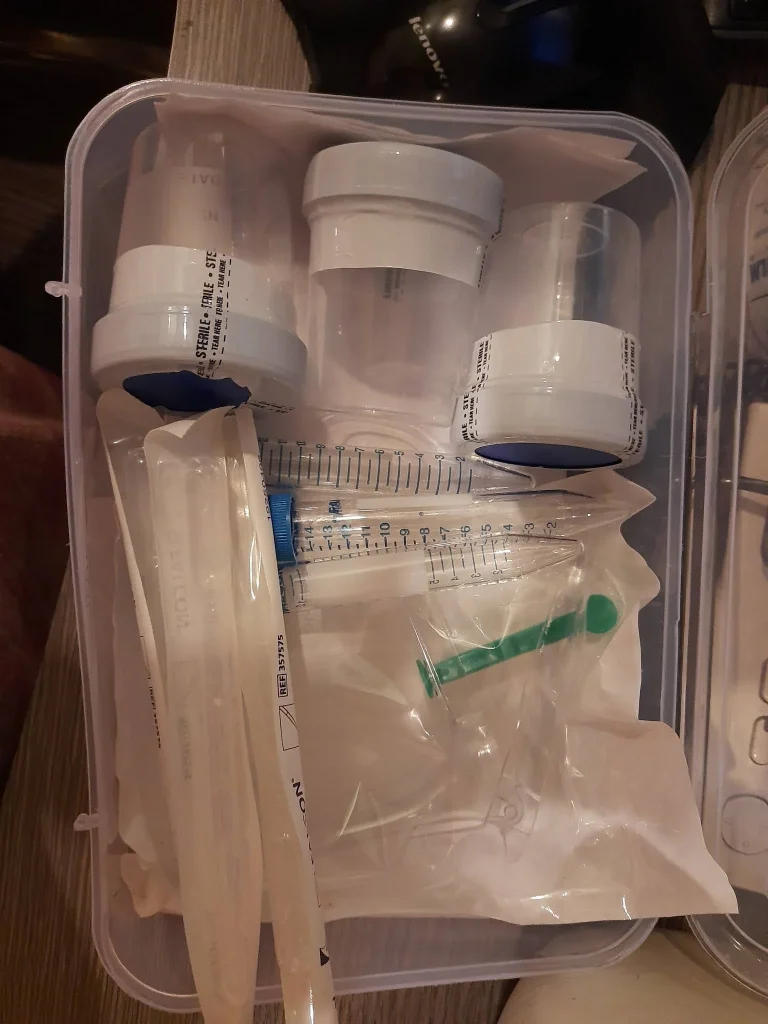
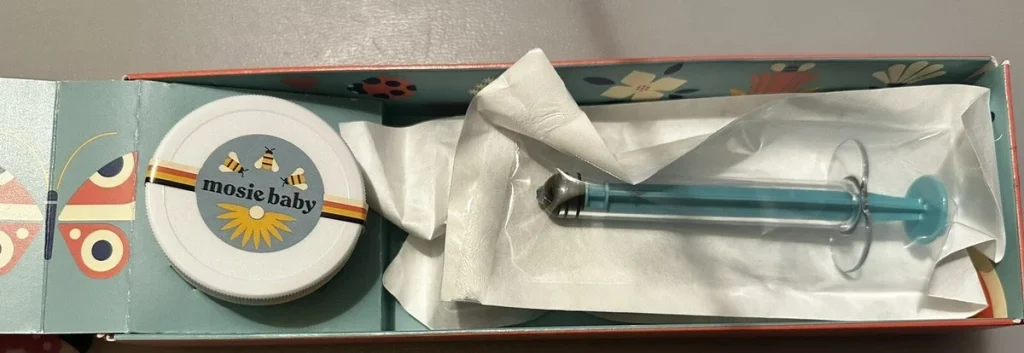
4) Use a home insemination kit designed for ICI
A kit can help with controlled placement and reduce the “awkward scramble” feeling. If you’re comparing options, look for straightforward instructions and body-safe materials.
If you’re looking for a place to start, you can explore an at home insemination kit option and see whether it fits your plan and comfort level.
Safety and testing: What to think about before you try
At-home insemination should prioritize hygiene, consent, and health screening. This is where it helps to slow down and be methodical.
Hygiene basics
Use clean hands, clean surfaces, and follow product instructions. Avoid improvising with non-body-safe items. If something causes pain, stop and consider checking in with a clinician.
Donor screening and documentation
If you’re using a sperm bank, screening is typically part of the process. With a known donor, talk about STI testing and timing. Many people also discuss genetic carrier screening, though what’s appropriate varies by situation and budget.
Legal parentage: don’t assume “we’re all friends” is enough
Legal headlines have underscored a tough reality: in some places, at-home donor arrangements can create parentage questions later. Laws vary widely. If you’re using a known donor, it’s worth talking to a family-law attorney in your jurisdiction before you begin, even if everyone is aligned emotionally.
Tech tools are helpful, but keep them in perspective
Apps can make tracking easier, and people increasingly lean on algorithm-driven predictions. If you’re curious about how these tools “think,” you can read about the home insemination kit—and then remember that your body is not a spreadsheet. Use tools for support, not self-judgment.
Medical disclaimer: This article is for general education and is not medical advice. It does not diagnose, treat, or replace care from a licensed clinician. If you have pelvic pain, irregular bleeding, known fertility conditions, or questions about testing and medications, consult a qualified healthcare professional.
FAQ: Quick answers people are asking right now
Is ICI the same as IVF?
No. ICI places sperm in the vagina near the cervix, while IVF fertilizes eggs in a lab and transfers an embryo.
Do I need a doctor to try at-home insemination?
Not always, but medical guidance can help if cycles are irregular, you’ve been trying for a while, or you have known health concerns.
What’s the difference between ICI and IUI?
ICI is vaginal placement (often at home). IUI is uterine placement (usually in a clinic) and may be recommended in certain cases.
How many days should we try ICI?
Many people focus on the fertile window around ovulation. Tracking can help narrow timing, and clinicians can advise on individual factors.
What legal issues matter with known donors?
Parentage rules vary, and at-home arrangements can carry legal risk. Consider legal advice and written agreements before trying.
CTA: Choose a plan that protects your peace
If you’re exploring ICI, aim for a setup that supports your relationship (or your emotional bandwidth, if you’re doing this solo). Clear timing, clear consent, and a kit that reduces chaos can make the experience feel more grounded.