Is a home insemination kit actually a realistic IVF alternative for some people?
What do you do if the “trying” part feels more like a TV plot twist than a private moment?
And how do you make ICI at home feel clean, calm, and not overly clinical?
For many LGBTQ+ people and solo parents by choice, at-home insemination (ICI) sits in that in-between space: more accessible than clinic care for some, but still serious enough to deserve a plan. Pop culture keeps circling fertility storylines—actors’ pregnancies written into shows, buzzy new TV dramas about babies, and celebrity pregnancy chatter. Real life is less scripted. A simple, supportive setup can help you feel grounded.
Below is a decision-style guide for using a home insemination kit for ICI, with a focus on tools, technique, comfort, positioning, and cleanup. It’s not medical advice, and it can’t replace a clinician, but it can help you think clearly before you try.
A quick note before you start (the real-world context)
In recent news coverage, courts and lawmakers have been discussing how at-home insemination intersects with parental rights—especially when a donor is known and insemination happens outside a clinic. If you’re building your family with a known donor, it’s smart to treat the legal side as part of your “prep,” not an afterthought.
If you want a broad jumping-off point to read more, here’s a helpful place to start: Florida Supreme Court makes ruling in at-home artificial insemination case.
The choose-your-path decision guide (If…then…)
If you want a lower-intervention home option… then consider ICI first
ICI usually aims to place semen near the cervix using a syringe-style applicator. It doesn’t require a clinic procedure, and many people like that it can be done in a familiar space with a partner, a friend, or solo support.
If you’re comparing ICI to IVF, think of ICI as “start simple” rather than “same outcome.” IVF is a medical pathway with monitoring, retrieval, and lab fertilization. ICI is a home technique that may be appropriate for some bodies and situations, and not for others.
If timing feels stressful… then simplify your tracking and protect your mood
Plenty of people start with apps and strips and end up feeling like they’re managing a mini election night map of hormones. If that’s you, scale down. Pick one tracking method you trust, and build a small buffer for rest and privacy.
If you’re using frozen sperm, timing and handling matter even more. Follow the sperm bank’s instructions closely, and don’t be afraid to ask questions before the day-of.
If you’re using a known donor… then treat consent and parentage as part of “setup”
At-home conception can be emotionally intimate and legally complicated at the same time. Recent headlines have underscored that in some places, donors may later seek legal recognition, even when everyone began with a different understanding.
If you’re working with a known donor, consider getting legal guidance in your state (or country) before you try. Agreements, clinic involvement, and local parentage rules can change the risk picture.
If your main goal is comfort… then build a “soft landing” plan
ICI can feel vulnerable. A comfort plan keeps it from turning into a sterile scene change between commercials.
- Warm the room: A towel, a pillow, and a calm playlist can matter more than people admit.
- Set expectations: Decide ahead of time whether you want conversation, silence, or a quick check-in.
- Protect privacy: Put phones on do-not-disturb and pre-stage anything you’ll need.
If you’re wondering about positioning… then choose steady over acrobatic
You don’t need a dramatic, reality-TV confessional-level setup. Many people choose a comfortable recline with hips slightly supported (like with a pillow) because it feels stable and reduces immediate mess.
Pick a position you can hold without strain. Tension can make the moment harder than it needs to be.
If cleanup is your biggest anxiety… then prep like you’re hosting yourself
Cleanup is often the part no one talks about until it’s too late. Make it easy on future-you.
- Lay down a towel and keep tissues nearby.
- Wear a liner or period underwear afterward if leakage would spike your stress.
- Plan the next 30 minutes (water, snack, show) so you’re not rushing around immediately.
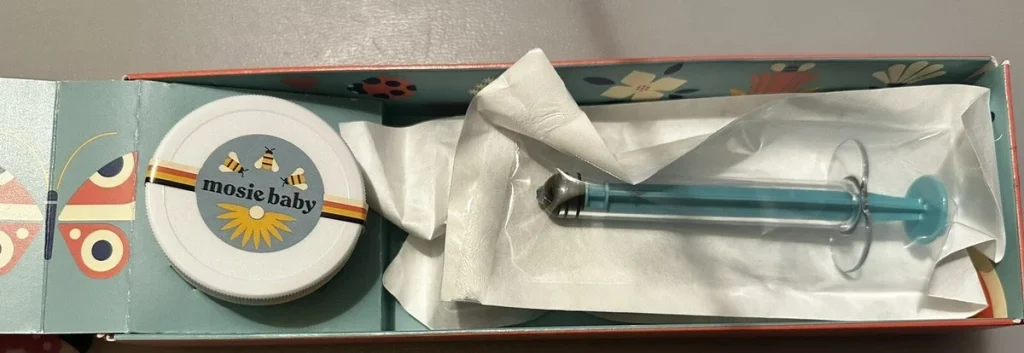
If you’re choosing tools… then use purpose-made, body-safe supplies
The goal is gentle, controlled placement—not improvisation. A purpose-built option can reduce discomfort and help you feel more confident about hygiene and handling.
If you’re shopping, start with a product designed for at-home ICI, like an at-home insemination kit for ICI.
If you’ve tried a few cycles without success… then consider when to bring in a clinician
Home options can be empowering, but they’re not the only path. If you’re feeling stuck, overwhelmed, or unsure about timing, it may help to consult a fertility clinician for testing and next-step options. That could include monitored cycles, IUI, or IVF, depending on your situation and goals.
FAQ (quick answers)
Is ICI the same as IUI?
No. ICI is typically done at home and places semen near the cervix. IUI is a clinic procedure that places washed sperm into the uterus.
How long should I rest after insemination?
Rest for comfort and calm. There isn’t one proven rest time for everyone, so choose a short window that helps you relax.
Can I do ICI if I’m using frozen sperm?
Often yes, but follow thaw and handling instructions precisely. When in doubt, ask the sperm bank or a clinician for guidance.
What should I avoid using as an applicator?
Avoid non-sterile, non-body-safe tools. Choose supplies intended for insemination to reduce irritation and infection risk.
Do laws treat at-home insemination differently than clinic conception?
Sometimes. Recent reporting has highlighted parentage disputes tied to at-home insemination in certain jurisdictions. A local family-law professional can help you understand your risk and options.
Call to action: make your next try feel simpler
If you’re aiming for a calm, practical home attempt, focus on what you can control: the right tools, a comfortable setup, and a cleanup plan that doesn’t derail your day.
How does at-home insemination (ICI) work?
Medical disclaimer: This article is for general educational purposes only and does not provide medical or legal advice. Fertility choices are personal and can involve health and legal considerations. For individualized guidance, consult a qualified clinician and, when relevant, a family-law attorney in your area.












