Navigating Conception After Birth Control: A Partner’s Guide
When a couple decides they are ready to start a family, navigating conception after birth control can be a daunting and confusing process. Birth control, whether it be the pill, patch, or other method, can have a significant impact on a woman’s body and reproductive system. As a partner, it’s important to understand the potential effects of birth control and how to support your partner in their journey towards conception. In this blog post, we will discuss the various factors to consider when trying to conceive after being on birth control, as well as offer tips for supporting your partner during this time.
Understanding the Effects of Birth Control on the Body
Before delving into how to navigate conception after birth control, it’s important to understand the potential effects that birth control can have on a woman’s body. Depending on the type of birth control used, it may take some time for the body to regulate and return to its natural menstrual cycle. The pill, for example, contains synthetic hormones that prevent ovulation, and it can take a few months for the body to adjust and start ovulating again. Other birth control methods, such as the Depo-Provera shot, can take up to a year for fertility to return to normal.
Additionally, birth control can also have an impact on a woman’s cervical mucus, which plays a crucial role in conception. Some forms of birth control can thicken the mucus, making it difficult for sperm to reach the egg. It’s important to keep these factors in mind when trying to conceive after using birth control.
Timing is Everything
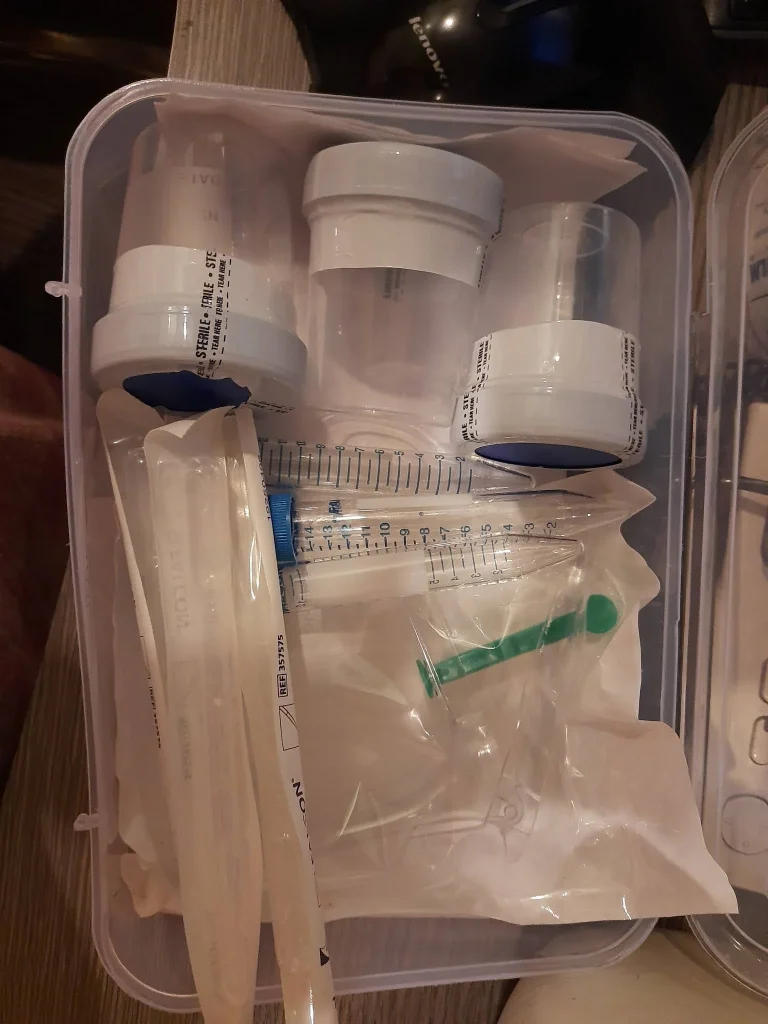
One of the most important factors in conceiving after birth control is timing. As mentioned earlier, it can take some time for a woman’s body to regulate after stopping birth control, so it’s crucial to track ovulation and have sex during the most fertile days of the cycle. There are various methods for tracking ovulation, such as using ovulation predictor kits or tracking basal body temperature, but it’s important to find the method that works best for your partner.
It’s also important to keep in mind that fertility can vary from month to month, even for women who have regular cycles. It may take a few months of tracking to determine the most fertile days, so patience and consistency are key.
Supporting Your Partner
Navigating Conception After Birth Control: A Partner's Guide
Trying to conceive after birth control can be emotionally and physically draining for both partners. As a partner, it’s important to be supportive and understanding during this time. Here are some ways to support your partner:
1. Be patient: It may take some time for your partner’s body to regulate after stopping birth control. Be patient and understanding if it takes longer than expected to conceive.
2. Communicate openly: Talk to your partner about their feelings and concerns. It’s important to have open and honest communication during this process.
3. Offer emotional support: Trying to conceive can be a rollercoaster of emotions, and your partner may need extra emotional support during this time. Be there to listen and offer a shoulder to lean on.
4. Educate yourself: Take the time to educate yourself about birth control and its potential effects on the body. This will not only help you understand what your partner is going through, but it will also help you provide better support.
5. Be involved: Attend doctor’s appointments and fertility treatments with your partner. This shows your support and involvement in the process.
6. Take care of yourself: It’s important to take care of yourself during this time as well. Trying to conceive can be stressful, so make sure you are taking care of your own physical and emotional well-being.
In conclusion, navigating conception after birth control can be a challenging process, but with understanding and support from their partner, it can be a smoother journey. It’s important to educate yourself about the potential effects of birth control and to be patient and supportive during this time. With proper timing and communication, you and your partner can successfully navigate conception after birth control and start your journey towards parenthood.
Summary: When a couple decides to start a family, navigating conception after birth control can be overwhelming. Birth control can have significant effects on a woman’s body and fertility, and it’s important for partners to understand and support each other during this time. Timing is crucial in trying to conceive after birth control, and communication and patience are key in supporting one another. By educating themselves and being actively involved, partners can successfully navigate this journey towards parenthood.








