- Timing beats perfection: a simple fertile-window plan often matters more than fancy extras.
- Don’t let trends run your cycle: social media “pre-pregnancy” hype can add stress without adding clarity.
- PCOS and busy schedules are real: sleep shifts, desk jobs, and stress can make ovulation harder to predict.
- Keep supplies body-safe: use the right tools for comfort and to protect sperm quality.
- Know when to get help: if timing is solid and it’s not happening, a clinician can help you choose next steps.
Between celebrity bump speculation, TV-storyline fertility twists, and election-season debates about reproductive rights, it can feel like everyone has an opinion about how pregnancy “should” happen. Real life is quieter and more practical: you want a plan that fits your body, your schedule, and your family-building path.

This guide focuses on ICI (intracervical insemination) using a home insemination kit—with an emphasis on timing and simplicity. It’s LGBTQ+ inclusive, donor-friendly, and built to reduce guesswork.
Medical disclaimer: This article is educational and not medical advice. It can’t diagnose conditions (including PCOS) or replace care from a licensed clinician. If you have pain, repeated pregnancy loss, very irregular cycles, or known fertility concerns, consider professional guidance.
Overview: where at-home ICI fits in right now
At-home insemination is part of a bigger conversation. People are juggling demanding workdays, inconsistent sleep, and stress that can ripple into cycles—topics that come up often in PCOS and fertility discussions. At the same time, headlines about court cases and state-by-state policy changes remind many families to think ahead about logistics, privacy, and paperwork.
ICI at home is a lower-intervention option than clinic procedures like IUI or IVF. For some, it’s a first step. For others, it’s a way to build a family with a known donor or a partner’s sperm in a comfortable setting.
Timing: the fertile-window plan that doesn’t take over your life
If there’s one “secret,” it’s this: your goal is to get sperm close to the cervix during the fertile window. You don’t need a complicated spreadsheet. You do need a consistent method.
Start with two signals, not five
Pick two tracking signals and use them together:
- LH ovulation tests (urine strips): helpful for catching the surge.
- Cervical mucus changes: often becomes clearer, stretchier, and wetter as ovulation approaches.
- Basal body temperature (BBT): confirms ovulation after it happens (useful for learning your pattern).
If you have PCOS or irregular cycles, LH tests can be confusing for some people. Pairing them with mucus observations and cycle history can make timing feel less like a coin flip. If you repeatedly can’t identify ovulation, a clinician can help you troubleshoot safely.
A simple timing approach (general guidance)
Many people plan insemination around peak fertile signs:
- Option A (1 attempt): on the day of the LH surge/peak fertile signs.
- Option B (2 attempts): one attempt the day you see a surge/very fertile mucus, and another about 12–24 hours later.
- Option C (3 attempts): add an earlier attempt when fertile mucus first appears (useful when ovulation timing is unclear).
Frozen sperm often has a shorter window after thaw than fresh sperm. If you’re using frozen donor sperm, ask your bank or clinician for timing guidance specific to your situation.
A note on “trimester zero” planning
You may have seen viral content pushing intense preconception rules. Some clinicians have cautioned against turning “planning” into pressure. If a trend makes you anxious or rigid, it’s not helping your fertility journey. Choose a few supportive habits—sleep consistency, manageable movement, balanced meals, stress reduction—and keep it livable.
Supplies: what you actually need (and what to skip)
At-home ICI works best when you keep the setup clean, comfortable, and body-safe.
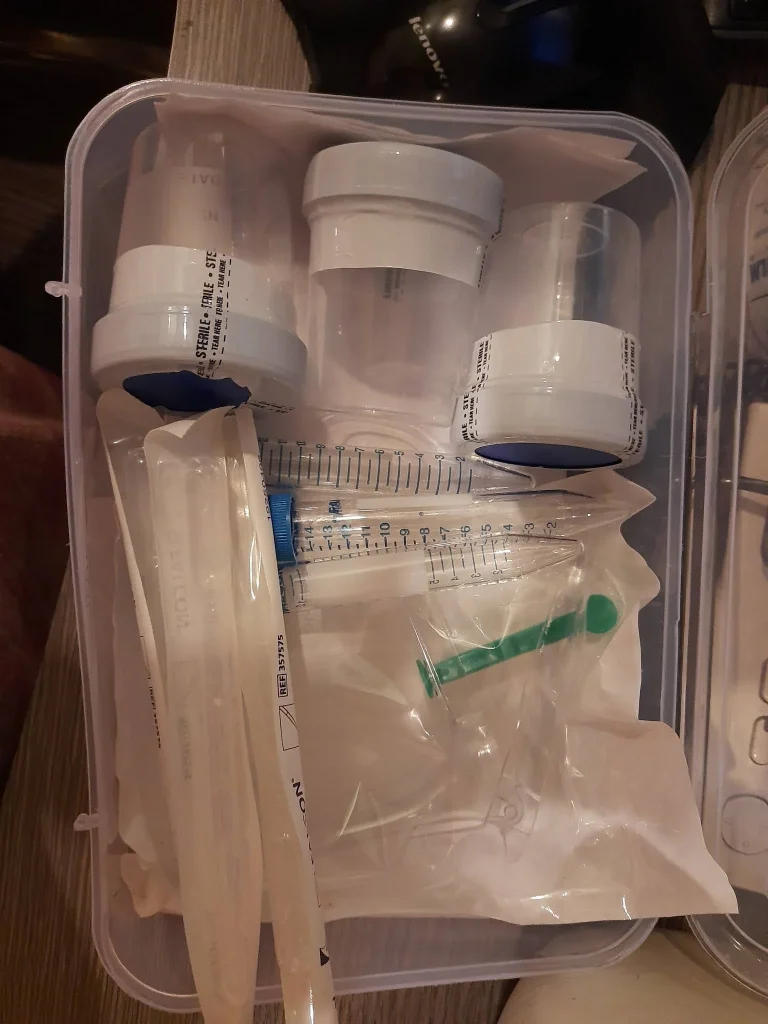
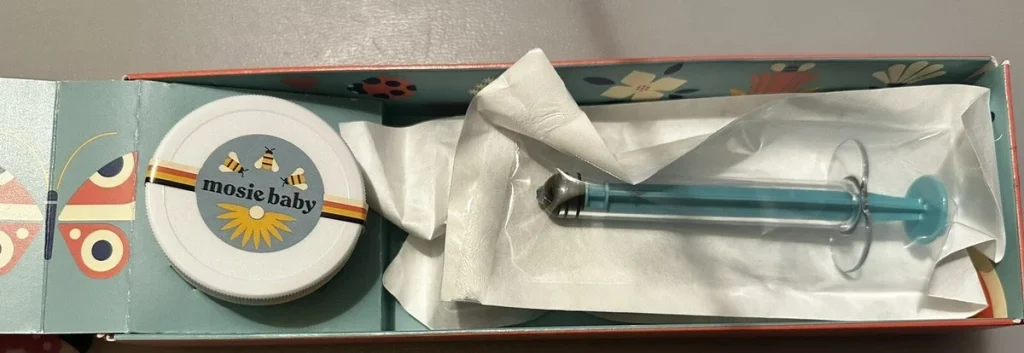
Essentials
- Home insemination kit designed for ICI (body-safe syringe/applicator and collection tools as needed).
- Clean, private space and a timer/clock.
- Optional comfort items: pillow for hip support, water-based lubricant that is fertility-friendly (avoid products that can harm sperm unless labeled sperm-safe).
Skip these common “hacks”
- Household syringes or improvised tools not intended for the body.
- Oil-based lubricants or saliva (can be sperm-unfriendly).
- Anything scented or “warming.” Comfort should never sting.
If you’re curious how tech is shaping fertility tracking apps and predictions, it helps to understand the basics of the home insemination kit. Still, remember: an algorithm can’t see your real-time biology the way your body signs and tests can.
Step-by-step: a clear ICI routine at home
This is a general, non-clinical walkthrough. Follow the instructions that come with your kit, and consult a clinician if you have pain, bleeding, or a medical condition that changes what’s safe for you.
1) Prep the space and wash hands
Set out supplies, wash hands thoroughly, and aim for a calm environment. Stress doesn’t “ruin” a cycle, but a relaxed setup can make the process easier and more consistent.
2) Collect or prepare the sample (as applicable)
Use the collection method recommended by your kit and sperm source. Keep everything clean and avoid exposing the sample to heat or harsh chemicals. If you’re working with frozen sperm, follow thaw instructions exactly.
3) Load the applicator slowly
Go slowly to reduce air bubbles and spills. If your kit includes a specific design to minimize loss, use it as directed.
4) Get into a comfortable position
Many people choose to lie on their back with hips slightly elevated. Comfort matters more than acrobatics. Pick a position you can repeat next cycle without dread.
5) Place semen near the cervix (ICI)
Insert the applicator gently into the vagina and deposit the sample near the cervix. Stop if you feel sharp pain. Mild pressure can be normal; pain is a signal to pause and reassess.
6) Stay resting briefly, then resume your day
Rest for a short period if it feels helpful. Leakage afterward can happen and doesn’t automatically mean the attempt failed. The goal is placement at the right time, not “keeping everything in.”
Mistakes that quietly lower your odds (and easy fixes)
Mistake 1: Over-trusting calendar predictions
Fix: Use LH tests and/or cervical mucus to time attempts in the moment. If your cycles vary, a calendar alone often misses the window.
Mistake 2: Turning tracking into a stress marathon
Fix: Choose two tracking methods and stick with them for a few cycles. Consistency beats intensity.
Mistake 3: Using the wrong lubricant or untested supplies
Fix: Stick to body-safe tools and sperm-friendly lubricant (or none). Avoid DIY devices.
Mistake 4: Ignoring the bigger context (logistics and rights)
Fix: If you’re using donor sperm or planning co-parenting, consider learning about local rules and paperwork early. With ongoing public attention to reproductive rights litigation and state policy differences, planning ahead can reduce last-minute stress.
FAQ: quick answers for common ICI questions
Is ICI painful?
It shouldn’t be sharply painful. Gentle pressure can happen. Stop if you feel significant pain, dizziness, or bleeding, and seek medical advice.
Do I need to orgasm for it to work?
No. Some people find it relaxing, but it’s not a requirement for conception.
How long should we try before changing plans?
It depends on age, cycle regularity, and health history. If you’re not sure, a clinician can help you decide when to add testing or consider options like IUI/IVF.
Next step: choose a kit that matches your timing-first plan
If you want a simple setup designed for comfort and less mess, consider an at-home insemination kit for ICI. The best kit is the one you can use confidently, on the right days, without turning your home into a lab.
However you’re building your family—solo, partnered, with a known donor, or with banked sperm—you deserve information that feels steady. Keep it timing-first, keep it body-safe, and let your plan support your life (not swallow it).