Myth: At-home insemination is a “wild west” DIY shortcut.

Reality: With the right screening, clean supplies, and clear documentation, ICI can be a practical home fertility option for many solo parents and LGBTQ+ families. It’s not a replacement for medical care, but it can be a meaningful first step before more intensive paths.
Overview: Why people are talking about ICI right now
Fertility conversations have been everywhere lately—from wellness trends like meditation for stress support, to renewed attention on reproductive policy and court battles, to a growing market for supplements. Add in the constant drumbeat of celebrity pregnancy rumors and plotlines in new TV dramas, and it’s no surprise people are asking what options exist outside a clinic.
At-home insemination (ICI) often comes up as a lower-intervention alternative to IVF for some situations. It can also be a bridge option while you’re waiting on appointments, saving money, or deciding what level of medical involvement feels right.
Timing: Your cycle is the schedule (not the internet)
Timing does more heavy lifting than almost anything else with ICI. That’s why ovulation calculators and home ovulation tests keep trending—people want clarity, not vibes.
How to find your fertile window
- Ovulation tests (LH strips): Helpful for catching the surge that often happens shortly before ovulation.
- Cervical mucus: Many people notice more slippery, stretchy mucus near ovulation.
- Cycle tracking: Apps and calendars can help you spot patterns, but they’re estimates.
If you’re using frozen sperm, timing tends to be less forgiving than with fresh. If anything about timing feels confusing, ask your sperm bank or clinician for guidance.
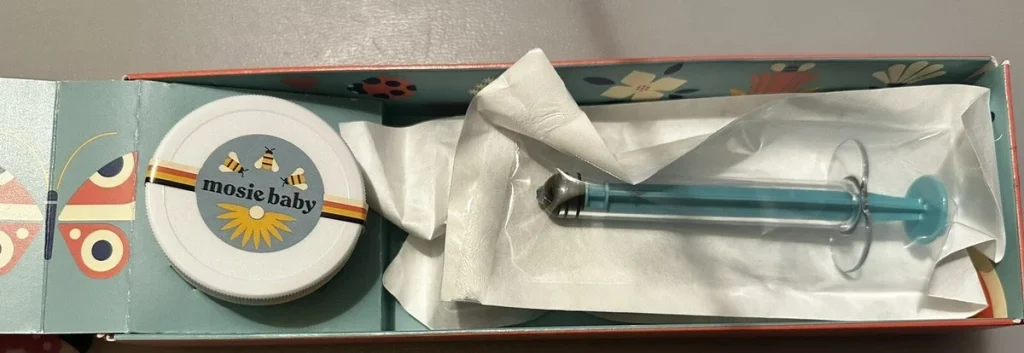
Supplies: What a home insemination kit should cover
Think “clean, simple, single-use.” A home insemination kit is mainly about using the right tools and reducing avoidable risk.
Core items to have ready
- Needleless syringe(s): Designed for insemination (no needles).
- Collection container: Clean and appropriate for semen collection.
- Optional: A speculum if you’ve been taught to use one safely (many people skip this).
- Fertility-friendly lubricant: Only if needed and labeled sperm-friendly.
- Clean setup: Soap and water, clean towels, and a stable surface.
Skip “hacks” from social media. If a tip sounds like a movie plot device, it probably doesn’t belong in your conception plan.
Step-by-step: A practical ICI routine (at home)
This is a general, non-clinical overview. If you have pain, bleeding, known pelvic conditions, or a history that raises infection risk, talk with a clinician before trying at home.
1) Confirm consent and your plan
Before you start, align on boundaries and expectations—especially with a known donor. Write down what you agreed to and store it somewhere safe.
2) Prep a clean, calm environment
Wash hands thoroughly. Lay out supplies. Keep pets out of the room and reduce distractions. If stress is high, consider a short breathing or mindfulness routine; people often explore meditation for coping, even though outcomes vary.
3) Collect and handle semen safely
- Use the collection container provided or a clean, appropriate container.
- Avoid saliva, lotions, or non–fertility-friendly lubricants.
- If using fresh semen, follow your kit guidance on timing between collection and insemination.
4) Draw into the syringe slowly
Go slowly to reduce bubbles. Keep everything as clean as possible. Use single-use items and don’t set tips down on questionable surfaces.
5) Inseminate near the cervix (ICI)
Get into a comfortable position. Insert the syringe gently into the vagina (not the uterus) and release contents slowly. Pain is a stop sign, not something to push through.
6) Give it a little time
Many people choose to remain lying down briefly afterward. There’s no perfect number of minutes, but a calm pause can help you reset emotionally.
7) Document the attempt
Write down the date, timing relative to ovulation testing, and any notes. This helps you learn what works and supports your records if legal questions ever arise.
Common mistakes that waste cycles (or add risk)
- Guessing ovulation: Use LH tests and body signs instead of hoping you “nailed it.”
- Using non-sterile tools: Reusing syringes or containers can increase infection risk.
- Skipping donor screening: STI testing and clear agreements matter, even when everyone trusts each other.
- Assuming supplements are a shortcut: Demand is rising, but “popular” doesn’t always mean “proven for you.”
- Ignoring burnout: High stress and overwork can affect libido, sleep, and follow-through. Protect your energy like it’s part of the protocol.
Safety, screening, and legal basics (especially with known donors)
Reproductive policy and court decisions have kept family-building in the spotlight. That attention is a reminder to plan for both health and legal clarity.
Health screening to consider
- Recent STI testing for anyone providing semen (and for the person trying to conceive, as recommended).
- Clear handling instructions for frozen sperm from the bank or clinic.
Legal risk reduction
- Use written agreements and keep copies of communications.
- Learn your state’s parentage rules before you start. A short consult with an LGBTQ+-affirming family lawyer can prevent major stress later.
FAQ: Quick answers before you order supplies
If you’re comparing tools or tracking methods, remember that some apps now use predictive features that sound “smart.” If you’re curious about the broader concept behind those tools, see home insemination kit.
CTA: Choose a kit that keeps things clean and simple
If you’re ready to build a safer setup at home, start with supplies designed for ICI instead of improvised tools. Consider an at-home insemination kit for ICI that prioritizes hygiene and ease of use.
How does at-home insemination (ICI) work?
Medical disclaimer: This article is for general education and is not medical or legal advice. It does not diagnose, treat, or replace care from a qualified clinician. If you have pelvic pain, abnormal bleeding, fertility concerns, or questions about STI screening or parentage, seek guidance from an appropriate healthcare professional and/or attorney.