Before you try… run this quick checklist.

- Timing plan: OPKs (ovulation tests), cervical mucus tracking, or a clinic-monitored cycle.
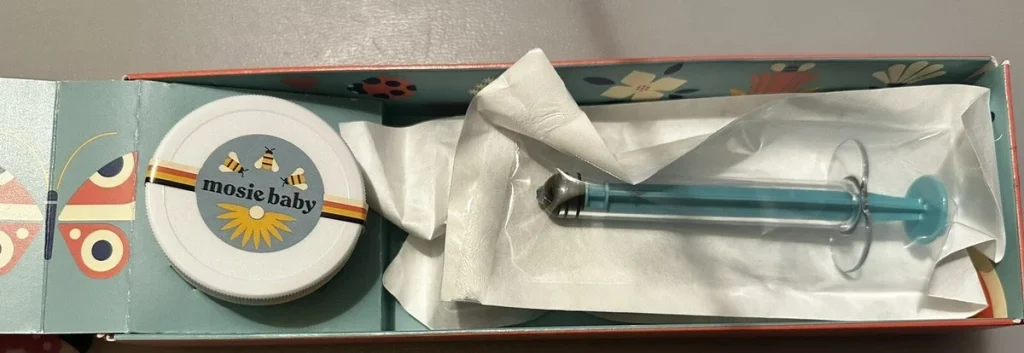
- Supplies: a clean home insemination kit, a specimen cup (if using fresh), towels, and a timer.
- Comfort: pillows, a calm playlist, and a “no rushing” window.
- Consent + roles: who preps, who inseminates, who handles cleanup, and how you’ll pause if anyone feels overwhelmed.
- Backup plan: what you’ll do if the timing feels off or the sample isn’t usable.
Big picture: why ICI is getting so much attention right now
Fertility talk is everywhere lately. News coverage about more people becoming first-time parents later in life has reignited the “35” conversation, and it can land like a ticking clock. The more accurate framing is less dramatic: fertility doesn’t fall off a cliff on a birthday, but it can change over time, and it’s influenced by more than one body.
That cultural noise shows up in everyday life too. A celebrity pregnancy headline, a twisty TV storyline, or a book-to-screen romance with surprise-family themes can make it feel like everyone else has a neat, linear path. Real life is messier. That’s one reason at-home ICI appeals to many solo parents and LGBTQ+ families: it can be a practical first step before jumping to clinical options.
ICI is not a replacement for medical care when you need it. Still, for some people it’s a reasonable starting point, especially when cycles are predictable and there’s no known infertility diagnosis.
The feelings part: pressure, privacy, and the two-week wait
Trying at home can be empowering, and it can also be emotionally loud. The same space where you decompress after work becomes the place where you test, track, and hope. If you’re using donor sperm, there can be extra layers: cost per vial, shipping logistics, and the weight of “don’t waste this try.”
It helps to name what you want the attempt to feel like. Some people want it clinical and efficient. Others want it intimate. Many want both, depending on the day. Decide in advance what “support” looks like—silence, jokes, a snack, a debrief, or zero discussion until tomorrow.
If you’re partnered, try a quick check-in script: “Do you want coaching, company, or quiet?” It reduces misunderstandings when nerves are high.
Practical steps: a simple ICI flow that doesn’t overcomplicate it
1) Get your timing as close as you reasonably can
With ICI, you’re aiming to place semen at the cervix around ovulation. Many people use ovulation predictor kits (OPKs) to catch the LH surge. Others combine OPKs with cervical mucus changes or basal body temperature tracking. If your cycles are irregular, timing can be trickier, and that’s a good moment to consider professional guidance.
If you’re using frozen sperm, timing often matters even more because the viable window after thaw can be shorter than with fresh samples. Follow the sperm bank’s handling instructions closely.
2) Set up the space like you’re about to paint a room
You don’t need a spa vibe, but you do want a clean, organized station. Lay out what you’ll use, wash hands, and keep pets out of the room for a few minutes. Think “calm and contained,” not “perfect.”
3) Positioning: choose comfort over gymnastics
Most people do best lying on their back with hips slightly elevated on a pillow. Side-lying can also work if that’s more comfortable. The goal is steady placement near the cervix, not acrobatics. If you’re tense, your body will tell you—slow down and reset.
4) The insemination itself: slow, steady, and gentle
Use a syringe-like applicator designed for insemination rather than improvised tools. Insert gently, then depress the plunger slowly to help reduce leakage and cramping. Afterward, many people stay reclined for 10–20 minutes. That time can be quiet, sweet, or purely practical.
5) Cleanup and aftercare
Expect some fluid to come back out when you stand up. That’s normal and not a sign the attempt “failed.” Use a pad if you want, hydrate, and do something grounding. Some people like a short walk; others like a shower and a show.
Safety and testing: what to prioritize before you try
Use the right tools and keep them clean
Choose a kit intended for at-home insemination. Avoid sharp edges, reusable items that can’t be properly cleaned, or anything not meant for body-safe use.
Know your sample source and screening
Donor sperm is typically screened through a sperm bank process, but policies vary by country and clinic. If you’re using a known donor, talk through STI testing, timing for results, and agreements in writing. Many families also consult a legal professional about parentage and consent, especially with known-donor arrangements.
A note on semen quality and storage
Research discussions often mention motility (movement) and vitality (live sperm) as helpful indicators when evaluating samples, including after storage. The practical takeaway for at-home tries is simple: follow handling instructions, minimize delays, and keep timing tight around ovulation.
When to pause and seek medical help
Get medical support if you have severe pain, fever, unusual discharge, heavy bleeding, or a history that suggests you may need tailored care. If you’re trying for multiple cycles without success, a clinician can help assess ovulation timing, sperm factors, and whether IUI or IVF might offer better odds.
Medical disclaimer: This article is for general education and is not medical advice. It can’t diagnose conditions or replace care from a licensed clinician. If you have symptoms, known reproductive conditions, or questions about medications, testing, or treatment, consult a qualified healthcare professional.
FAQs people are asking about ICI at home
Is ICI the same as IVF?
No. ICI places semen at the cervix using a syringe-like applicator, usually at home. IVF involves lab fertilization and clinical procedures.
Does fertility drop exactly at 35?
Not overnight. Many people notice changes over time, and age is only one factor. Sperm factors, cycle regularity, and health history also matter.
How many times should we try ICI in a cycle?
Many people try once around ovulation, while others do two attempts spaced about a day apart. If you’re using limited donor vials, a clinician can help you plan.
Can ICI work with frozen donor sperm?
It can, but timing is especially important because thawed sperm may have a shorter window. Ask the bank about vial type and recommended use.
What lubricant is safe to use during insemination?
If you need lube, look for fertility-friendly options that are labeled sperm-safe. Avoid products that are not designed for conception attempts.
When should we consider getting medical support?
Consider support if you have very irregular cycles, known reproductive conditions, significant pain/bleeding, or multiple unsuccessful cycles—especially if time feels tight.
Next step: choose a kit that supports a calm, controlled attempt
If you want a purpose-built option, start with a at-home insemination kit for ICI that’s designed for comfort and control. And if you’re curious about how modern tools can shape health conversations more broadly, you might also look up home insemination kit for a plain-language overview.