- Timing beats intensity: one well-timed try can matter more than a perfect “routine.”
- ICI is about placement, not pressure: comfort and a steady hand usually win.
- Pop culture isn’t real life: TV surprise pregnancies make great plot twists, not reliable expectations.
- Age talk is everywhere: headlines debate “cliffs,” but fertility is more like a slope with lots of individual variation.
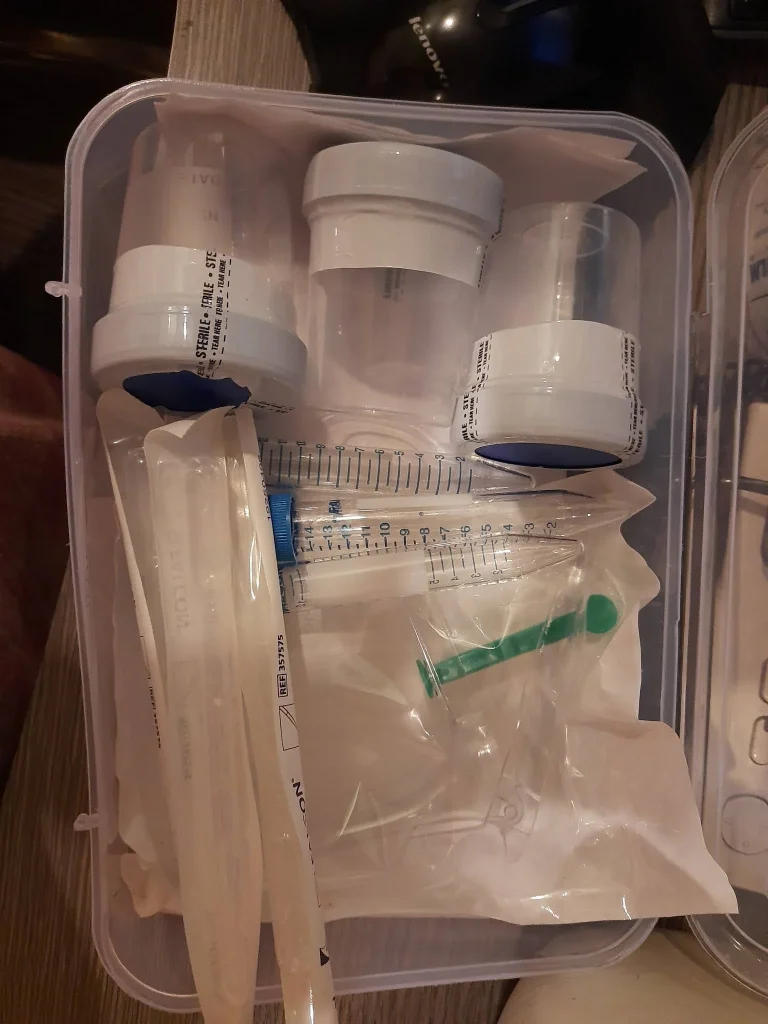
- Tools help: a home insemination kit + ovulation tracking can make trying at home feel less like guesswork.
What’s trending: fertility timelines, TV pregnancies, and the “cliff” debate
Right now, the cultural conversation about getting pregnant is loud. You’ll see think pieces questioning whether a “fertility cliff” really hits at 35, and you’ll also see entertainment coverage dissecting how often a real actor’s pregnancy gets written into a show. Add in a new tear-jerker TV drama about babies and family-making, and it’s easy to feel like everyone else is moving faster than you.

Meanwhile, practical tools are getting attention too. Ovulation calculators and at-home ovulation tests keep popping up in roundups, because they give you something concrete to do in a process that can feel abstract.
If you’re exploring ICI (intracervical insemination), you’re not alone. Many LGBTQ+ people, solo parents, and couples using donor sperm choose at-home insemination as a first step before jumping to medicated cycles or IVF.
What matters medically (without the hype)
Timing basics: egg lifespan vs sperm lifespan
For most people who ovulate, the egg is available for a short window after ovulation. Sperm can sometimes survive longer in fertile cervical mucus. That’s why the days leading up to ovulation and ovulation day itself often get the most attention.
Ovulation calculators can estimate your fertile window based on past cycles. Ovulation predictor kits (OPKs) look for an LH surge, which often happens shortly before ovulation. Using both can reduce “we missed it” anxiety.
A note on age—yes, including the sperm side
Age gets framed as a single deadline, but fertility usually changes gradually. Headlines often focus on the egg side, yet research conversations also include sperm. One recent research headline discussed how increasing age in men can be linked with changes in sperm quality and DNA integrity, while pregnancy outcomes in assisted reproduction may not track in a simple, one-to-one way.
Takeaway: if you’re using a partner’s sperm or a known donor, it can be worth thinking about overall sperm health and timing strategy, not just calendar age. If you’re using banked donor sperm, you may have limited vials, which makes timing and technique even more important.
Medical disclaimer
This article is for general education and support. It isn’t medical advice and can’t diagnose or treat any condition. If you have pain, unusual bleeding, known fertility concerns, or questions about infections or donor screening, talk with a qualified clinician.
How to try at home: an ICI playbook focused on tools + technique
Step 1: Set up your space (comfort counts)
Choose a private spot where you won’t feel rushed. Gather what you need before you start: your home insemination kit, a clean towel, and any tracking info (OPK result, calendar estimate). If you’re using frozen sperm, follow the sperm bank’s thaw guidance exactly.
A simple rule: aim for calm, not clinical. If your body tenses, insertion can feel harder than it needs to.
Step 2: Positioning that’s practical
Many people prefer lying on their back with knees bent, similar to inserting a tampon. Others find a side-lying position more comfortable. There’s no single “magic angle.” Pick what helps you relax and keep the syringe steady.
Step 3: Placement for ICI (the goal)
ICI places semen near the cervix, not into the uterus. Go slowly, insert only as far as comfortable, and depress the plunger steadily. A gentle pace can reduce cramping and helps avoid spills.
After insemination, staying reclined for 10–20 minutes can feel reassuring. It’s not a guarantee, but it may help you stay relaxed and avoid immediate leakage from standing up quickly.
Step 4: Cleanup and what’s normal afterward
Some leakage is common. Semen and cervical fluid don’t all stay in place, and that doesn’t mean the attempt “failed.” Mild cramping can happen. Severe pain, fever, or foul-smelling discharge is not typical—seek medical care if those occur.
Step 5: Timing strategy that fits real life
If you’re using OPKs, many people plan ICI around the first positive test and again the next day, depending on sperm availability. If you have only one vial, you may choose a single attempt timed as close as possible to your surge/ovulation estimate.
If you’re a data person, you might notice how much fertility tracking resembles pattern-finding. People even compare it to tech tools that “learn” from signals—though bodies aren’t algorithms. If you’re curious about the concept, here’s a general explainer on home insemination kit.
Looking for a purpose-built option? Explore an at home insemination kit for ICI that’s designed for comfort and control.
When to seek extra support (and what “help” can look like)
At-home ICI can be a reasonable first step, but it’s not the only step. Consider talking with a fertility-aware clinician if cycles are irregular, ovulation is unclear, or insemination is consistently painful. It’s also smart to get guidance if you have endometriosis, PCOS, a history of pelvic infections, or known low sperm counts.
Many people also check in after several well-timed cycles without a positive test, especially when using limited donor vials. Support can range from basic lab work and ultrasound timing to medicated cycles, IUI, or IVF—depending on your situation and goals.
FAQ
Is ICI the same as IUI?
No. ICI places semen at the cervix using a syringe. IUI is done in a clinic and places washed sperm into the uterus.
How many days should we try ICI in a cycle?
Many people try 1–3 attempts around the LH surge and the day after, but timing depends on your cycle and sperm source.
Do we need to orgasm or keep hips elevated after insemination?
Neither is required. Lying down for 10–20 minutes can feel reassuring, but pregnancy is mostly about timing and sperm meeting the egg.
Can we use an ovulation calculator and ovulation tests together?
Yes. A calendar-style predictor can help you plan, while LH tests can confirm when your surge is happening that cycle.
When should we talk to a clinician?
Consider it if you have irregular cycles, known fertility conditions, repeated losses, or if you’ve tried for several cycles without success—especially if age is a factor for either partner.
Next step: make your next try feel simpler
If you’re ready to try ICI at home, focus on two things you can control: timing and a calm, clean setup. The rest—celebrity bump chatter, TV plotlines, and internet debates—can stay in the background.