On a Tuesday night, “Rae” paused a streaming drama mid-episode. A character’s pregnancy had suddenly become a major plotline, and it felt oddly familiar. Everywhere Rae looked, there were celebrity bump updates, “is she or isn’t she?” headlines, and roundups of actors whose real-life pregnancies were written into shows. Meanwhile, Rae was staring at a calendar and thinking: I just want one solid plan that doesn’t waste a cycle.
If that’s you, you’re not alone. Pop culture makes pregnancy look like a surprise twist. In real life, many people—straight, LGBTQ+, solo parents by choice—want a practical path they can control. For some, that means exploring at-home insemination (ICI) with a home insemination kit as a lower-intervention alternative before jumping to clinic-based options like IUI or IVF.
The big picture: where at-home ICI fits in 2026 fertility talk
Between celebrity pregnancy announcements and entertainment lists about storylines adapting to real pregnancies, it’s easy to feel like everyone is “just getting pregnant.” That can be motivating, and it can sting. It also can push people toward rushed decisions.
At-home ICI sits in the “doable, real-life” lane. It’s often discussed alongside other fertility options because it can be more accessible, more private, and more budget-friendly than starting with a full clinic cycle. It’s not a replacement for medical care when you need it. Still, it can be a reasonable first step for people with predictable cycles and no known fertility barriers.
One more modern layer: tools that promise to optimize everything. From ovulation calculators to apps using pattern detection, people are trying to turn conception into a clean formula. If you’re curious how that tech thinking is framed broadly, here’s a plain explainer on home insemination kit. Just remember: fertility tracking tools can be helpful, but they’re not magic, and bodies aren’t plotlines.
The emotional side: hope, pressure, and the “headline effect”
Celebrity news can create a weird kind of urgency. One day it’s a glowing announcement. The next day it’s speculation and denial stories. If you’re trying, it can feel like the whole world is watching a scoreboard you didn’t agree to join.
At-home ICI can feel empowering because you choose the setting and the pace. It can also feel tender. Many people carry a mix of excitement and fear: fear of “doing it wrong,” fear of disappointment, fear of spending money and time without results.
It helps to name the goal for your next attempt. Not “get pregnant this cycle or else.” Instead: “Give ourselves a clean, well-timed try.” That mindset protects your nervous system and keeps decision-making clearer.
Practical steps: a cycle-saving ICI plan (without the overwhelm)
This is a general education overview, not medical advice. If you’re using donor sperm, follow the bank’s instructions carefully and consider clinic guidance for thawing/handling when applicable.
1) Pick your tracking method (simple beats perfect)
To avoid wasting a cycle, timing matters more than fancy extras. Choose one or two methods you’ll actually use:
- Ovulation predictor kits (OPKs): Often used to catch the LH surge that typically happens before ovulation.
- Cervical mucus changes: Many people notice more slippery, egg-white-like mucus near ovulation.
- Calendar + past cycles: Useful if your cycles are consistent.
2) Decide on your timing window
Many people aim for ICI the day before ovulation and/or the day of ovulation. If you’re using OPKs, a common approach is to inseminate after a positive test, then consider a second attempt the next day if you have the resources and your plan allows.
If you’re working with limited vials or limited donor access, plan your “best shot” day in advance. That prevents last-minute scrambling, which is how cycles get wasted.
3) Prep your space like you’re hosting “future you”
Comfort helps your body relax, and relaxation helps the experience feel sustainable across cycles. Set up:
- Clean hands and a clean surface
- Good lighting (less fumbling)
- A towel and tissues
- A pillow to support hips if that’s comfortable
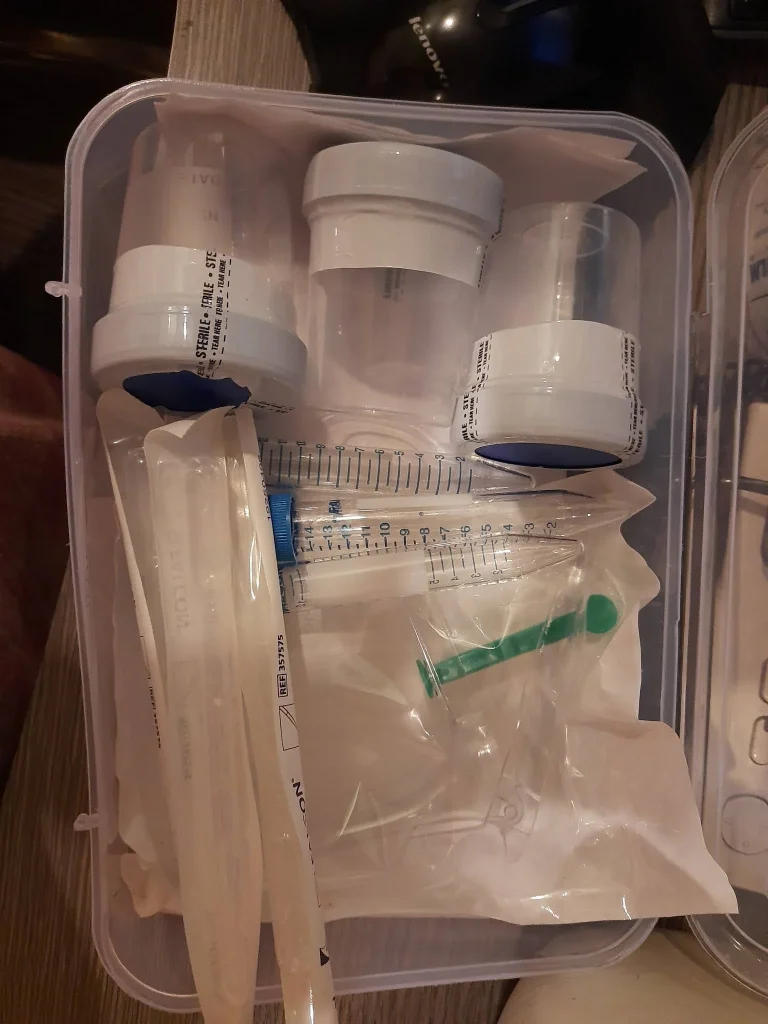
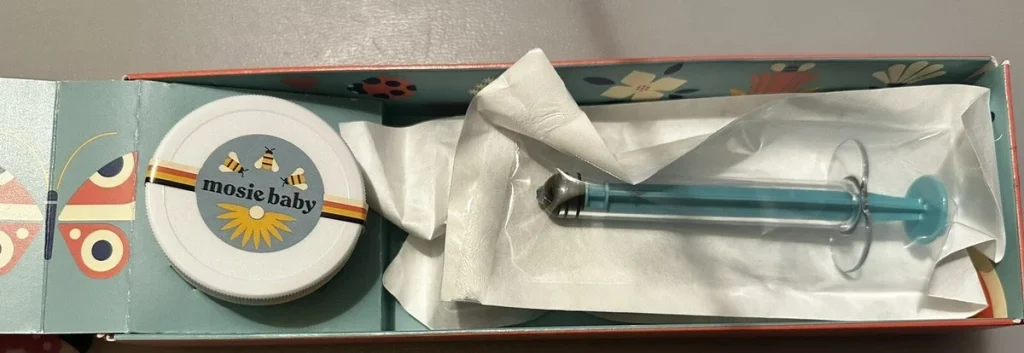
4) Use a kit designed for the job
A at-home insemination kit for ICI is typically designed to help place semen at the cervix more effectively than improvised tools. The goal is a calmer process with less mess and less guesswork.
Avoid using sharp objects, anything not meant for the body, or products that can irritate vaginal tissue. If you’re unsure whether a lubricant is sperm-friendly, skip it unless it’s clearly labeled as fertility-friendly.
5) Keep the aftercare simple
Many people choose to lie down for a short period after insemination. The bigger win is reducing stress and avoiding unnecessary “rituals” that add pressure. If cramps, dizziness, fever, or unusual pain occurs, seek medical advice.
Safety and testing: what matters most (especially with donor pathways)
Safety isn’t about being anxious. It’s about being intentional.
Donor source and screening
If you’re using donor sperm, consider how screening and handling will be managed. Banked sperm is typically tested and quarantined under established protocols. Known-donor arrangements vary widely, and testing plus clear consent are important.
Consent and legal clarity
For LGBTQ+ families and known-donor situations, legal parentage can be as important as timing. Laws differ by location. If possible, consult a qualified attorney familiar with family-building in your area before insemination—especially if more than two adults are involved in planning or parenting.
When to loop in a clinician
Home ICI is not the right fit for every body or every history. Consider medical support if cycles are irregular, if you suspect ovulation issues, if you’ve been trying for a while without success, or if you have symptoms that concern you.
Medical disclaimer: This article is for general education and is not medical advice. It does not diagnose or treat any condition. For personalized guidance—especially around fertility, medications, infections, or pregnancy loss—talk with a licensed clinician.
FAQ: quick answers before you try
Is ICI the same as IVF?
No. ICI places sperm at the cervix, while IVF involves fertilization in a lab and embryo transfer. Many people try ICI first because it’s simpler and often less expensive.
When is the best time to do ICI at home?
Most people aim for the day before ovulation and/or the day of ovulation. Ovulation predictor kits and cycle tracking can help you narrow the window.
Can LGBTQ+ couples use a home insemination kit?
Yes. Many queer couples, solo parents, and trans people use at-home ICI with donor sperm. The best approach depends on your body, donor source, and legal considerations.
Do I need a clinic to use donor sperm?
Not always. Some people use banked, tested donor sperm, while others use a known donor. Testing, consent, and local legal guidance matter either way.
What are signs I should talk to a clinician before trying at home?
Consider getting medical guidance if you have irregular cycles, known reproductive health conditions, repeated unsuccessful cycles, severe pain, or a history of pregnancy loss.
Ready for a calmer, less wasteful attempt?
If your goal is a clean, well-timed try at home—without turning your cycle into a full-time job—start with a plan you can repeat. Choose your tracking method, pick your best day, and use tools designed for ICI.