On a Tuesday night, “Maya” (not her real name) paused a streaming drama right as the plot hit a pregnancy twist. Her group chat was already buzzing—celebrity baby rumors, a politician’s soundbite about “family values,” and a friend’s screenshot of a new movie trailer where everyone seems to be expecting. Maya muted the noise and opened her notes app instead: “ICI at home. What’s safe? What’s real? What do we do next?”

If you’re in a similar place—curious about at-home insemination (ICI), looking for an IVF alternative, or trying to keep costs and logistics manageable—you deserve a plan that’s calm, inclusive, and grounded in risk reduction. Below is a decision guide built around “if…then…” branches, with extra attention to screening, consent, and documentation.
Medical disclaimer: This article is educational and not medical advice. It can’t diagnose or treat fertility conditions. If you have pain, abnormal bleeding, known fertility factors, or questions about infections, medications, or timing, talk with a qualified clinician.
A decision guide for ICI at home (use the “if…then” branches)
If you want the simplest at-home path, then start with ICI basics
ICI (intracervical insemination) typically means placing sperm near the cervix during your fertile window. Many people choose it because it’s private, less clinical, and often less expensive than clinic-based options.
If you’re comparing it to IVF, remember the tradeoff: IVF brings lab support and more monitoring, while ICI depends heavily on timing, sperm quality, and your individual fertility factors.
If you’re considering a donor outside a clinic, then prioritize screening and consent
Headlines have recently spotlighted DIY insemination and “gray market” sperm arrangements, including legal disputes that can arise when screening and paperwork are unclear. Even when everyone has good intentions, informal setups can create medical and legal uncertainty.
If you’re using donor sperm, then aim to reduce risk by thinking through:
- Infection screening: Ask what testing is current, what was tested, and how results are shared.
- Identity and expectations: Clarify contact preferences, boundaries, and future communication.
- Legal parentage planning: Consider getting jurisdiction-specific legal advice before you try, especially for LGBTQ+ families and non-traditional arrangements.
To see why this is in the news, you can read more context via this search-style link: Home inseminations and gray market sperm: Florida Supreme Court case meets DIY fertility.
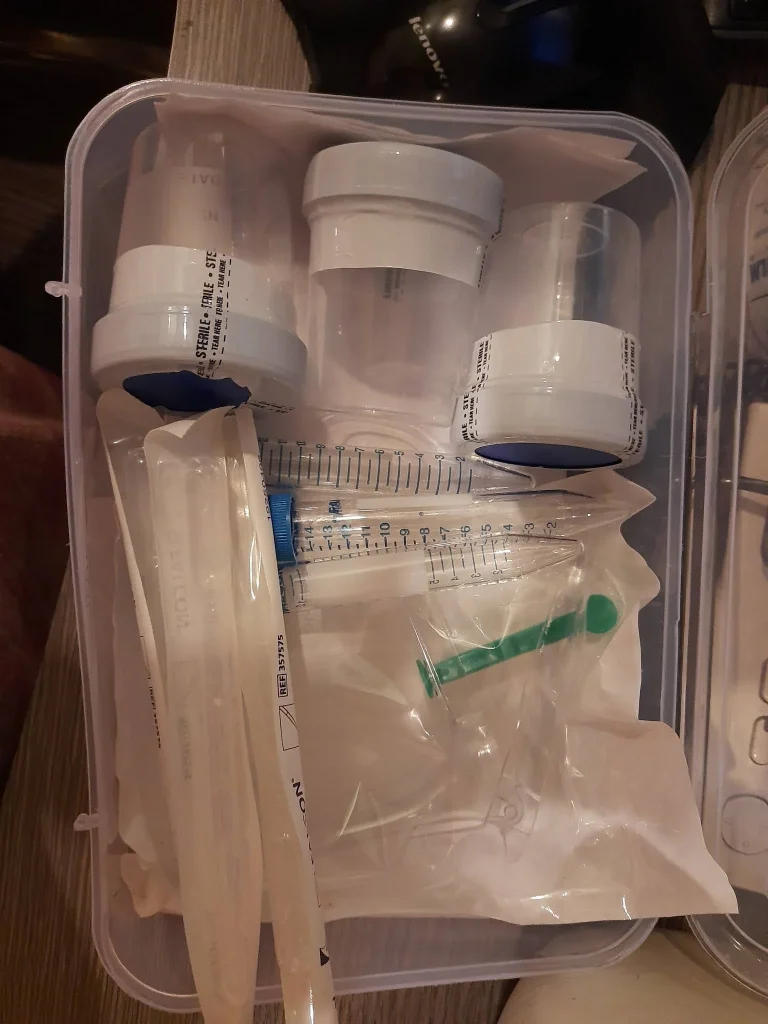
If safety is your top priority, then choose supplies designed for insemination
If you’re shopping for a home insemination kit, focus on tools meant for this purpose and a process that supports cleanliness. The goal is to reduce avoidable irritation and infection risk, and to help you feel confident that you did what you could within an at-home approach.
If you want a starting point, explore an at-home insemination kit for ICI that’s designed for home use.
If timing feels overwhelming, then build a “good enough” routine
Trying to conceive can turn your calendar into a command center. If you’re tracking, then keep it sustainable: a method you can actually follow beats a perfect plan you abandon mid-cycle.
If you’re not sure where to begin, consider a simple approach such as observing cycle patterns and focusing insemination attempts around your likely fertile days. For personalized timing advice—especially with irregular cycles—clinician guidance can help.
If stress and sleep are taking over, then treat support as part of the plan
People talk about fertility like it’s only hormones and timing, but your nervous system is part of the story. Recent clinical guidance and research discussions have highlighted stress during fertility treatment, and studies continue to explore how sleep disruption may relate to IVF outcomes.
If you’re doing ICI at home, then consider support moves that don’t require perfection: a consistent bedtime window, fewer late-night doomscroll sessions, and a check-in with a therapist or support group if you’re feeling depleted. Burnout is common in high-pressure careers too, and it’s increasingly part of the fertility conversation.
If you’re tempted by supplements, then slow down and verify quality
Market reports and trend roundups keep pushing “fertility supplements” into the spotlight. If you’re considering them, then treat them like any health product: look for third-party testing, read ingredient lists, and avoid stacking multiple products with overlapping vitamins or herbs.
If you have thyroid disease, PCOS, endometriosis, or you take prescription medications, then a clinician or pharmacist is the right place to sanity-check safety.
If you want an IVF alternative but need more support, then consider a step-up plan
At-home ICI can be a meaningful first step. Still, if you’ve tried several well-timed cycles without success, then it may be time to gather more information rather than just “try harder.”
If you want an in-between option, some people explore clinic testing, telehealth consults, or moving to IUI before IVF, depending on sperm source, age, cycle regularity, and known fertility factors. A clinician can help you choose the next rung on the ladder without jumping straight to the most intensive option.
A quick checklist to document choices (less drama later)
If you’re building a family outside traditional pathways, documentation can be a form of care. Consider keeping a private folder with:
- Donor screening information and dates (as available)
- Written agreements or expectations (even if informal)
- Receipts and kit details for your records
- Cycle notes (timing, symptoms, tests used)
If you plan to pursue legal parentage steps, then that folder can make your next conversation easier.
FAQs (fast answers)
Is ICI the same as IVF?
No. ICI places sperm near the cervix without lab fertilization. IVF fertilizes eggs in a lab and transfers an embryo.
Can you do ICI at home safely?
Many people try ICI at home, but safety depends on clean technique, appropriate supplies, and lower-risk donor pathways. Discuss STI testing and medical concerns with a clinician.
Why are people talking about “gray market” sperm?
News coverage has raised awareness that informal arrangements can skip screening, consent, and documentation, increasing infection and legal risks.
Do stress and sleep really matter for fertility?
They can influence overall reproductive health and how you experience treatment. Improving sleep and support can help you cope and stay consistent.
Should I take fertility supplements when doing ICI?
They’re popular, but quality varies. Choose third-party tested products and ask a clinician about interactions and appropriate dosing.
When should we consider switching from ICI to clinic care?
If you’ve tried multiple cycles, have irregular cycles, known fertility factors, or want testing and a clearer plan, a consult can help.
CTA: Choose clarity over chaos
If the cultural noise is loud—celebrity bump speculation, plotline pregnancies, and hot takes about who “should” be a parent—your plan can still be grounded and yours. Start with safety, screening, and documentation, then choose the level of support that matches your life.