Before you try at home insemination, run this checklist:
- Timing plan: How will you identify your fertile window (OPKs, cervical mucus, BBT, or a combo)?
- Sperm source: Banked, known donor with paperwork, or something informal? Know the tradeoffs before emotions kick in.
- Consent + boundaries: Who is involved, what contact is expected, and what happens if plans change?
- Relationship protection: How will you talk on hard days without turning it into blame?
- Backup step: If this cycle doesn’t work, what’s the next move—repeat, adjust timing, or consult a clinician?
At home insemination is having a cultural moment. It shows up in group chats, on reality TV storylines, and in that familiar celebrity-pregnancy rumor cycle where everyone pretends they’re an expert. Meanwhile, real headlines point to something less glamorous: legal and safety questions when people use informal or “gray market” sperm arrangements.
If you’ve been scrolling and thinking, “We could do this,” you’re not alone. This guide keeps it practical, inclusive, and relationship-aware—because the logistics matter, and so does how you treat each other while you try.
What people are reacting to right now (and why it matters)
When a court case or investigative story touches DIY fertility, it often centers on one theme: informal arrangements can collide with the legal system. It’s not just about biology. It’s about parentage, consent, documentation, and what happens when expectations differ later.
If you want a general starting point for the conversation that’s circulating, read this: Home inseminations and gray market sperm: Florida Supreme Court case meets DIY fertility.
On the more “consumer” side, the same moment includes lots of chatter about ovulation tracking accuracy, product testing roundups, and supplement demand. That mix can create pressure: it’s easy to feel like you’re one purchase away from certainty. You’re not. You’re building a process.
A decision guide: If…then… paths for real-life planning
If you’re choosing a sperm source, then decide how much risk you can carry
If you want the most predictable screening and paperwork, then consider a regulated sperm bank route. People often pick this for clearer medical screening and more defined documentation.
If you’re considering a known donor, then treat it like a relationship and a legal project, not a casual favor. Talk through expectations early: involvement, boundaries, future contact, and what “no” means at every step.
If you’re tempted by informal/gray market options because it feels faster or cheaper, then pause and price in the hidden costs: unclear testing, identity questions, and legal uncertainty. A family law attorney who understands assisted reproduction can be a strong investment, especially for LGBTQ+ families navigating parentage rules.
If timing is stressing you out, then simplify your tracking stack
If your cycles are fairly regular, then many people start with OPKs and one or two body signs. That can be enough to target the fertile window without turning your life into a spreadsheet.
If you’re testing constantly and spiraling, then set a boundary: pick specific times to test and a specific “stop time” for fertility talk each day. Anxiety loves unlimited access.
If your cycles are irregular or confusing, then consider getting clinical guidance sooner rather than later. You don’t need to “earn” help by suffering for months.
If the process is affecting your relationship, then name the pressure out loud
If one partner is carrying the mental load, then redistribute tasks. Let one person own timing; let the other own logistics (supplies, reminders, cleanup, or appointment research). Swap next cycle.
If sex and intimacy start feeling like performance reviews, then separate “trying” from “connecting.” Schedule a non-fertility date night. Protecting closeness is not optional; it’s part of sustainability.
If work burnout is part of the picture, then be honest about capacity. Some recent discussions in medical circles have highlighted how burnout and subfertility can intersect in complicated ways. You can’t white-knuckle your way into calm. Build rest into the plan.
If you’re picking tools for at-home insemination, then prioritize comfort and control
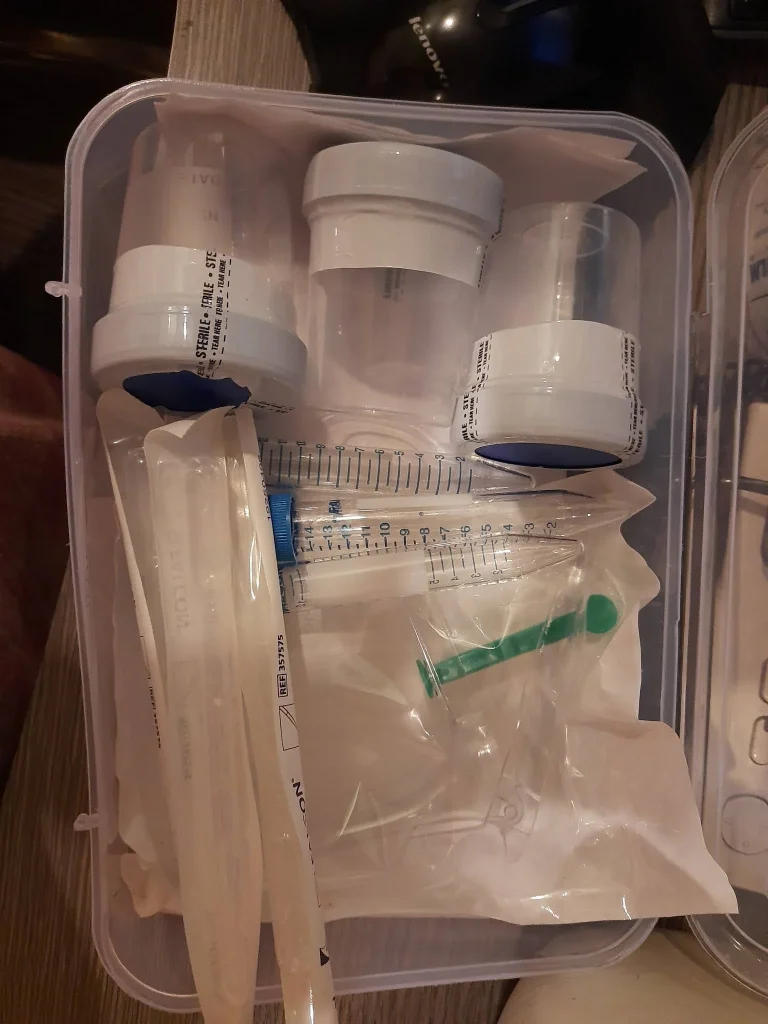
If you want a purpose-built option, then choose a kit designed for ICI and easy handling. A practical starting point is an at home insemination kit.
If you’re tempted to improvise with random supplies, then stop and reassess. Comfort, cleanliness, and predictability matter when emotions are already high. If you have questions about what’s safe for your body, ask a clinician.
Common communication snags (and quick resets)
Snag: “I’m doing everything right. Why isn’t it working?”
Reset: Replace certainty with curiosity. Try: “What’s one thing we can adjust next cycle without blaming either of us?”
Snag: One person wants more tries; the other wants a break.
Reset: Create a two-cycle agreement: one cycle “on,” one cycle “off,” then revisit. It prevents endless negotiation mid-stress.
Snag: Donor conversations feel awkward, so you avoid them.
Reset: Put it on the calendar. Avoidance doesn’t reduce risk; it just delays clarity.
FAQs
Is at home insemination the same as IUI?
No. At-home insemination usually means ICI (intracervical insemination). IUI is done in a clinic with sperm placed in the uterus by a clinician.
Do ovulation tests really help with timing?
They can. Many people use ovulation predictor kits (OPKs) plus body signs (like cervical mucus) to narrow the fertile window.
What are the biggest risks with “gray market” sperm?
Screening gaps, unclear identity/medical history, and legal uncertainty about parental rights can all be issues. Consider legal advice and safer sourcing.
How many tries should we do before getting help?
It depends on age, cycle regularity, and known fertility factors. If you feel stuck, or if there are pain/irregular cycles, a clinician can help you plan next steps.
Can stress and burnout affect fertility?
Stress doesn’t “cause infertility” in a simple way, but burnout can affect sleep, libido, cycles, and decision-making. Support and realistic pacing matter.
What should we talk about before we try?
Timing expectations, budget, donor boundaries, what “a good try” looks like, and how you’ll support each other if a cycle doesn’t work.
CTA: Make your next step calmer (not louder)
You don’t need perfect vibes or a perfect calendar. You need a plan you can repeat without losing yourselves in the process.
What is the best time to inseminate at home?
Medical disclaimer: This article is for general education and is not medical or legal advice. At-home insemination may not be appropriate for everyone. For personalized guidance—especially about infection risk, fertility conditions, medications, or parentage—talk with a qualified clinician and, when relevant, a family law attorney.