Before you try at-home insemination, run this quick checklist:
- Timing: You have a plan for tracking ovulation (LH strips, symptoms, or a monitor).
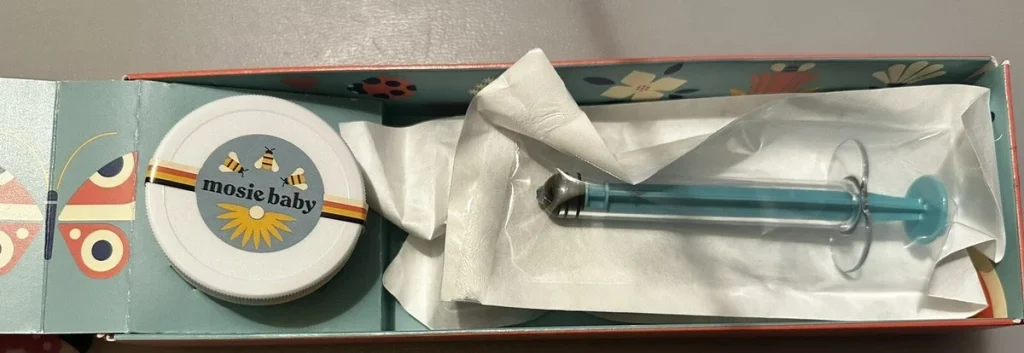
- Supplies: You’re using a home insemination kit designed for ICI—not improvised tools.
- Safety: You’ve thought through infection risk, donor screening, and clean handling.
- Documentation: You’ve saved receipts, donor paperwork (if applicable), and notes on timing.
- Plan B: You know when you’ll seek clinical support if cycles aren’t working.
Overview: Why ICI at home is trending in the conversation
Between celebrity pregnancy chatter, plotlines in TV dramas about “now or never” parenthood, and ongoing political headlines about reproductive healthcare access, it makes sense that more people are looking for options they can control at home. ICI (intracervical insemination) is one of those options: lower intervention than many clinic pathways, and often more accessible for LGBTQ+ family-building.
Another piece of the cultural noise right now is the idea of a “fertility cliff” at 35. Media takes can sound absolute, even when real life is more nuanced. If you’re feeling pressured by timelines, ICI can be a way to take action without jumping straight to IVF—while still keeping your next steps open.
Timing: The part that matters more than the vibe
If at-home insemination has a “make or break” factor, it’s timing. Your goal is to inseminate close to ovulation, when an egg may be available. Most people use ovulation predictor kits (OPKs) that detect the LH surge, then plan insemination shortly after.
Practical timing cues to consider
- OPK positive (LH surge): Many people try ICI the day of a positive test and/or the next day.
- Cycle tracking history: Past cycles can help you avoid starting OPKs too late.
- Cervical mucus changes: Some notice more slippery, “egg-white” mucus near ovulation.
Apps can help you organize information, but they estimate. Treat predictions as a starting point, not the final call.
Supplies: What to gather (and what to skip)
A calm setup reduces errors. It also helps you keep the process hygienic and consistent from cycle to cycle.
What’s typically helpful for ICI at home
- Home insemination kit: A purpose-built kit can improve control and comfort compared with improvised options.
- OPKs or an ovulation monitor: To narrow the window.
- Clean workspace: A freshly cleaned surface, good lighting, and a plan for disposal.
- Timer/clock: So you don’t rush the process.
- Notes app or journal: Record OPK results, insemination time, and any symptoms.
What to avoid
- Non-sterile tools: DIY devices can increase irritation or infection risk.
- Household lubricants: Some can be sperm-unfriendly. If you need lubricant, look for fertility-friendly options.
- Pressure-cooker “optimizations”: Overcomplicating the process can create more stress than benefit.
Step-by-step: A straightforward ICI flow at home
This is a general educational overview. Your exact steps may differ depending on sperm source (bank vs known donor), storage/transport, and any guidance you’ve received.
- Confirm your timing window. Use OPKs and your cycle history to identify your likely ovulation period.
- Wash hands and prep a clean area. Hygiene matters more than people think, especially when you’re focused on timing.
- Set up your supplies before you start. Open packaging only when you’re ready to use it.
- Get comfortable. Many people choose a position that supports easy access and relaxation.
- Perform ICI using your kit as directed. Go slowly. Gentle handling helps avoid irritation.
- Stay still briefly afterward. A short rest can help you feel settled and reduce immediate leakage.
- Document the attempt. Record the date/time, OPK result, and any relevant details (travel time, thaw time if applicable, etc.).
Mistakes to avoid: Safety, screening, and legal clarity
People often blame themselves when a cycle doesn’t work. Sometimes it’s simply biology and probability. Still, avoiding preventable pitfalls can protect your health and reduce regret.
1) Treating screening as optional
Whether you’re using a known donor or banked sperm, screening and safe handling reduce infection risk. If you’re unsure what’s appropriate for your situation, consider a conversation with a clinician or a fertility-focused counselor.
2) Skipping the paperwork when it matters
Headlines about shifting reproductive healthcare policies and court cases have made many families more documentation-aware. If you’re building your family with a donor pathway, keeping organized records can be helpful later. That may include donor agreements, bank documentation, receipts, and your cycle notes.
3) Letting supplement hype drive the plan
There’s a lot of market buzz about fertility supplements right now, including trend forecasts and growth reports. Supplements may have a role for some people, but they don’t replace ovulation timing, sperm handling, or medical care. If you take any, check interactions with a pharmacist or clinician—especially if you’re on other medications.
4) Over-relying on apps (or AI) for predictions
Tech can be useful, but it’s not magic. If you’re using tools that claim to “optimize” fertility timing, remember they’re still estimating based on inputs. For a broader lens on what AI is (and isn’t), see home insemination kit.
Choosing a home insemination kit: what to look for
Comfort and control matter. A kit designed for ICI can help you place semen near the cervix more reliably than improvised methods. Look for clear instructions, materials designed for body-safe use, and packaging that supports a clean setup.
If you’re comparing options, you can start here: at home insemination kit.
FAQs: quick answers before you try
Medical disclaimer: This article is for general education and is not medical or legal advice. It can’t diagnose conditions or replace care from a licensed clinician. If you have pain, unusual discharge, fever, a history of pelvic infection, or concerns about donor screening or legal parentage, seek professional guidance.
Next step: make your plan feel doable
At-home ICI works best when it’s treated like a simple, repeatable routine: track ovulation, keep things clean, and document what you did. That structure can reduce stress, especially when outside news cycles make reproductive decisions feel louder than they need to be.













