On a Tuesday night, “Maya” paused a streaming drama because a character’s pregnancy storyline felt a little too familiar. Not the glossy montage part—the real-life scramble: calendar tabs open, a box of supplies on the counter, and the quiet hope that this cycle won’t be a waste.

That mix of pop-culture fertility chatter (from TV plots to celebrity bump speculation) and real planning is everywhere right now. If you’re considering at-home insemination (ICI) with a home insemination kit, this guide keeps it practical, inclusive, and budget-minded—so you can focus your effort where it matters most: timing, prep, and a clean, calm process.
Big picture: where ICI fits among home fertility options
ICI (intracervical insemination) is an at-home method where semen is placed near the cervix during the fertile window. It’s often discussed as a lower-intervention option compared with clinic-based pathways like IUI or IVF.
People are also talking more about fertility “optimization” in general—apps, ovulation calculators, and a growing supplement market. Some tools can help you plan. Others mostly add noise. The goal here is a simple plan you can repeat without overbuying or overthinking.
Timing that protects your budget (and your energy)
If you only optimize one thing, make it timing. A perfectly executed attempt outside the fertile window is still a missed opportunity.
Find your fertile window without getting lost in apps
Many folks start with an ovulation calculator to estimate likely fertile days, then confirm with body signs or testing. Keep in mind: estimates are a starting point, not a guarantee, because stress, illness, travel, and sleep changes can shift ovulation.
Use ovulation tests as a “go-time” signal
Ovulation tests (OPKs) are popular because they’re straightforward: they detect a hormone surge that often happens shortly before ovulation. If you’re trying not to waste a cycle, OPKs can help you concentrate attempts into the most promising window.
If you’re using frozen donor sperm, timing matters even more because you may have fewer vials and a narrower margin for error.
A simple ICI timing approach many people use
- Start testing a few days before you expect to ovulate.
- Plan ICI around the day you see a positive OPK and/or the next day, depending on your pattern and sperm type (fresh vs. frozen).
- Track results (OPK day, cervical mucus notes, basal temp if you use it) to refine next cycle.
Medical note: timing advice can vary based on cycle length, irregular cycles, PCOS, postpartum cycles, and hormone use. If your cycles are unpredictable, a clinician can help you choose a monitoring approach.
Supplies: what you actually need (and what you can skip)
It’s easy to spend money on add-ons when you’re anxious. Keep your setup lean.
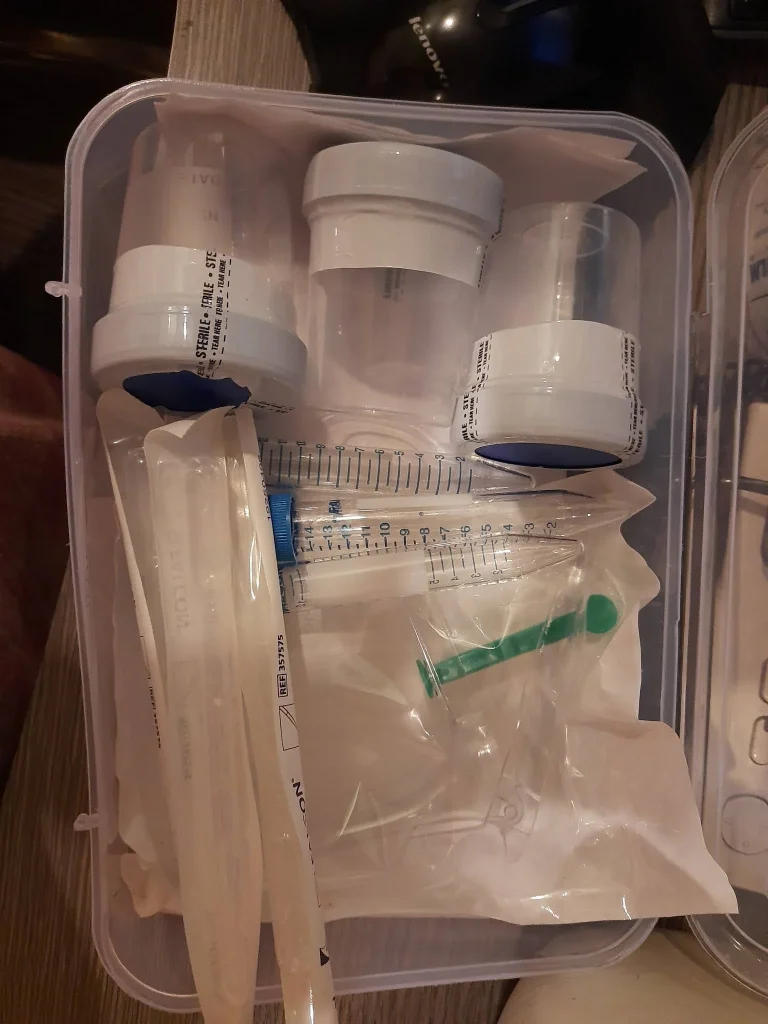
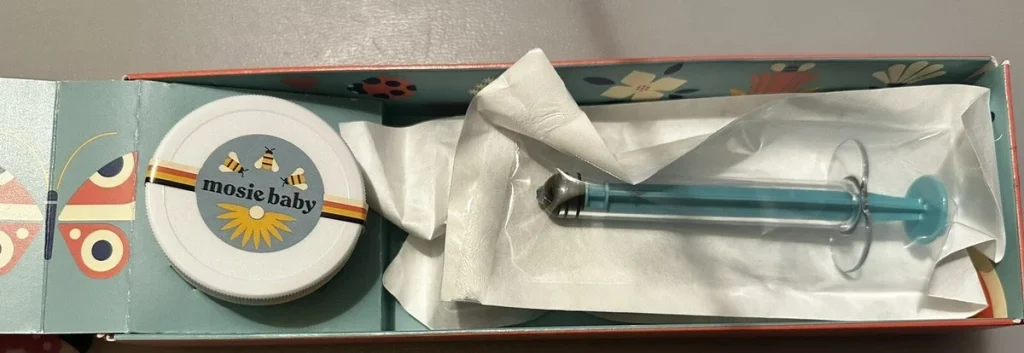
Core items for an ICI attempt
- Home insemination kit designed for ICI (with a syringe intended for this purpose).
- Ovulation tests (or another reliable method to identify the fertile window).
- Clean, private space and a timer/clock.
- Optional comfort items: lubricant that’s fertility-friendly (only if needed), a towel, and a pillow.
About “fertility supplements” and trend cycles
You may see headlines about rising demand for fertility supplements and next-year supplement trends. Some nutrients matter when there’s a deficiency, but supplements aren’t a shortcut to ovulation or a substitute for timing. If you’re considering a new supplement, check with a clinician or pharmacist—especially if you take other meds.
Step-by-step ICI at home (a calm, repeatable routine)
This is a general overview, not medical instruction. Always follow the directions that come with your kit and any guidance from your fertility clinic or sperm bank.
1) Set expectations and consent before the fertile window
If you’re trying with a partner, talk about roles (who preps, who tracks, who sets the mood, who wants quiet). If donor sperm is involved, confirm labeling, thaw guidance (if applicable), and any storage rules. Clarity now prevents last-minute stress later.
2) Prep your space like you’re setting up for a low-stakes procedure
Wash hands, clean the surface, and lay out everything you’ll use. Keep interruptions low. If you’ve been following the news about burnout and fertility strain—especially in high-pressure jobs—you already know that “calm” is not a vibe; it’s a plan.
3) Confirm timing
Use your chosen timing signals (OPK, cervical mucus, app estimate). If you’re unsure, it’s usually better to attempt a little earlier in the fertile window than after it has likely passed.
4) Inseminate per kit directions
Follow the kit’s steps for drawing up the sample and placing it at the cervix (ICI). Go slowly and gently. Discomfort is a sign to pause.
5) Give it a few minutes, then resume normal life
Many people rest briefly afterward for comfort and peace of mind. You don’t need an elaborate routine. Consistency across cycles helps you learn what works for your body and schedule.
Common mistakes that can waste a cycle (and how to avoid them)
Missing the window because the calendar “said so”
Apps predict; bodies decide. If your OPK and body signs disagree with the app, prioritize real-time signals.
Overcomplicating the process
When social feeds are full of “fertility hacks,” it’s tempting to add steps. More steps often create more chances for stress and errors. Keep the routine simple and repeatable.
Using the wrong products
Not every lubricant is sperm-friendly, and not every syringe is meant for insemination. Use products designed for this purpose and follow safety guidance.
Trying to power through burnout
Fertility planning can collide with demanding work and life. If you’re depleted, you’re not doing it wrong—you’re human. Build in small supports: a shared checklist, fewer attempts with better timing, and clear boundaries around fertility content.
FAQ: quick answers before you buy or try
Is ICI private?
It can be. Many people value the at-home setting, especially LGBTQ+ families and solo parents who want a calmer, more personal environment.
Can technology help with timing?
Yes, but choose tools that reduce confusion. Some apps now claim advanced prediction powered by data science. If you’re curious about the broader concept, see home insemination kit for context—then come back to basics: window + test + plan.
What if my cycles are irregular?
Irregular cycles can make timing harder. Consider combining OPKs with other signs, or talk with a clinician about monitoring options.
Ready to choose a kit and keep it simple?
If your goal is a practical, low-drama approach, start with the essentials and a clear timing plan. A purpose-built kit can help you avoid improvising with the wrong tools.
How does at-home insemination (ICI) work?
Looking for a starting point? Explore an at home insemination kit option and build a routine you can repeat without wasting a cycle.
Medical disclaimer: This article is for general education and does not provide medical advice, diagnosis, or treatment. If you have pain, fever, unusual symptoms, a history of pelvic infection, or questions about timing, medications, donor sperm handling, or fertility conditions, consult a qualified healthcare professional.