Fertility talk is everywhere right now. One minute it’s a TV drama rewriting a pregnancy storyline; the next it’s social media pushing a new “must-do” planning trend.

In real life, most people aren’t chasing hype. They’re trying to make a solid plan that doesn’t waste a cycle.
Thesis: A home insemination kit works best when you treat timing and setup like a simple, repeatable routine—not a last-minute scramble.
Overview: where at-home ICI fits (and where it doesn’t)
At-home insemination usually means ICI (intracervical insemination). It’s a lower-intervention option that some solo parents, LGBTQ+ couples, and people using donor sperm explore before moving to clinic-based steps.
It can feel like an “IVF alternative,” but it’s more accurate to call it a starting point. ICI won’t solve every fertility barrier, yet it can be a practical choice when your main goal is to get sperm close to the cervix at the right time.
Headlines also keep circling the same pressure points—age anxiety, “fertility cliff” debates, and trend-driven planning. If you’re feeling rushed by any of that, you’re not alone. Your best counter-move is a clear process you can repeat.
Timing: the part that saves (or costs) a cycle
If you’re budgeting donor sperm, timing matters as much as technique. One well-timed try can beat several poorly timed attempts.
Use signals you can actually track
- LH ovulation tests: Many people plan insemination around a positive LH surge.
- Cervical fluid: Slippery, clear, stretchy fluid can be a helpful sign for some bodies.
- Basal body temperature (BBT): Useful for confirming ovulation happened, not predicting it in advance.
If your cycles are irregular (common with PCOS), it can be harder to spot a surge. Stress, sleep disruption, and long desk-bound days can also affect cycles for some people. If your tracking feels like a constant mystery, a clinician can help you choose monitoring or medication options without jumping straight to IVF.
A simple window many people use
People often aim for one attempt around the LH surge and, if supplies allow, another within the next day. Your best plan depends on your cycle pattern and the type/quantity of sperm available.
Medical note: If you’re working with a sperm bank, follow their timing and thaw guidance. Some vials are labeled for clinical use only.
Supplies: what you need (and what’s just influencer clutter)
You don’t need a drawer full of gadgets. You need a clean, comfortable setup and a method that matches your sperm source.
The practical essentials
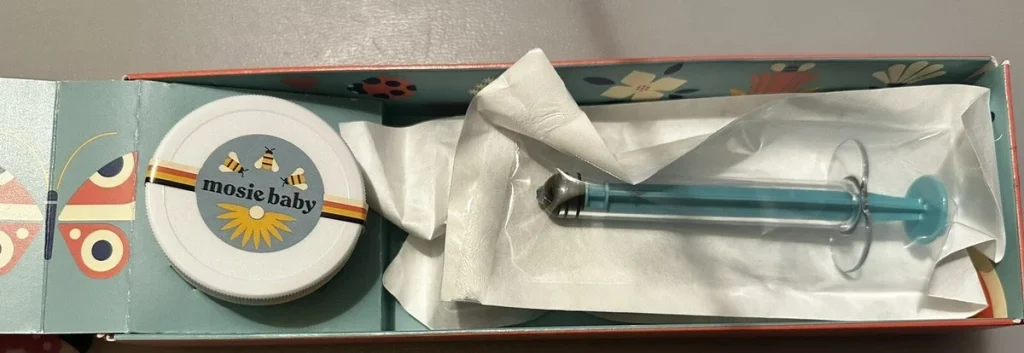
- Home insemination kit: A syringe designed for insemination (not a needle), plus a collection container if relevant.
- Ovulation tests: Enough to cover your likely fertile window.
- Clean, private space: Good lighting helps more than you’d think.
- Timer: For resting afterward and keeping the process calm.
Nice-to-have comfort items
- Water-based lubricant that’s fertility-friendly (avoid products that can be sperm-toxic).
- A pillow for hip support if that feels good to you.
- A heating pad for relaxation (not placed directly on the abdomen for long periods).
One modern twist: people are also using apps and predictions more than ever. Some even talk about algorithmic “fertility forecasting,” which can sound like magic. If you’re curious about the tech side of predictions, it helps to understand what home insemination kit actually means—patterns and probabilities, not guarantees.
Step-by-step: an at-home ICI routine you can repeat
This is general education, not medical advice. If you have pain, repeated infections, or known fertility conditions, get personalized guidance.
1) Set the scene before you start
Wash hands. Lay out supplies. Decide where you’ll place the kit afterward. Small prep steps reduce rushed mistakes.
2) Confirm your timing
Check your LH test result and your tracking notes. If you’re using frozen sperm, coordinate your plan with the thaw instructions so you’re not guessing under pressure.
3) Load the syringe carefully
Follow your kit’s directions. Avoid bubbles when possible, and keep everything clean. If anything touches an unclean surface, pause and reset with a new sterile item if available.
4) Inseminate slowly and gently
Get into a comfortable position. Insert the syringe only as directed by the product instructions, then depress the plunger slowly. Rushing can cause discomfort and doesn’t improve results.
5) Rest briefly, then carry on
Many people rest 10–20 minutes. Some notice leakage afterward; that’s common and doesn’t automatically mean it “didn’t work.”
6) Write down what happened
Log the time, LH result, any cervical fluid notes, and any issues with the process. This is how you get better without spending more.
If you’re choosing a kit, here’s a relevant option to explore: at-home insemination kit for ICI.
Common mistakes that waste a cycle (and how to dodge them)
Chasing trends instead of data
Some social platforms push “pre-pregnancy bootcamps” and strict timelines. If it spikes your anxiety, it can also derail consistent tracking. Keep your plan boring and measurable.
Testing too little (or too late)
If you only take one LH test per day, you can miss a short surge. Consider testing twice daily during your likely window if your cycles allow.
Using the wrong lubricant
Many common lubes can reduce sperm motility. If you use lube, pick one labeled fertility-friendly.
Not matching the plan to your sperm source
Fresh and frozen behave differently. Frozen sperm timing can be less forgiving, so coordination matters. When in doubt, ask the bank or a clinician for guidance.
Ignoring your body’s stress and sleep signals
Recent women’s health coverage keeps coming back to basics like sleep and stress. You can’t “wellness” your way out of every fertility barrier, but you can set up conditions that support consistent ovulation tracking.
FAQ: quick answers before you try
Is ICI painful?
It’s often described as uncomfortable at most, but bodies vary. Stop if you feel sharp pain or dizziness, and seek medical advice.
Can we do ICI without an orgasm?
Yes. Some people find arousal helps with comfort and cervical positioning, but it’s not a requirement.
How many cycles should we try before changing the plan?
It depends on age, diagnosis, sperm source, and how confidently you’re timing ovulation. If you’ve tried several well-timed cycles, a clinician consult can help you decide next steps.
CTA: make your next attempt calmer—and more efficient
If you want a simple, repeatable approach, start with a timing plan and a clean setup you can execute the same way each cycle. Consistency is a budget strategy.
How does at-home insemination (ICI) work?
Medical disclaimer: This article is for general educational purposes only and is not medical advice. It does not diagnose, treat, or replace care from a qualified clinician. If you have irregular cycles, PCOS, pelvic pain, recurrent infections, or concerns about donor sperm handling, consult a licensed healthcare professional.