Pop culture makes pregnancy look like a plot twist: a surprise bump written into a TV storyline, a whispered headline, a dramatic reveal before the credits roll.

Real life is quieter. It’s more about calendars, bodies, and choosing what feels doable this month.
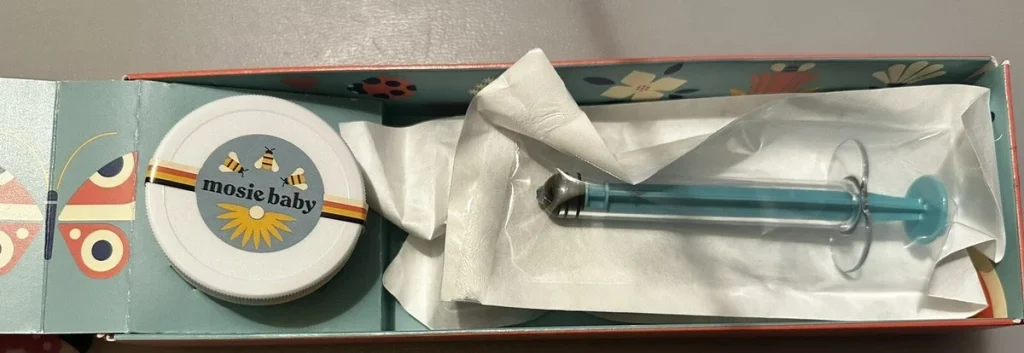
If you’re considering ICI, a home insemination kit can make the process feel more controlled, more private, and less clinical—without pretending timing and biology don’t matter.
What people are talking about right now (and why it hits home)
There’s a lot of cultural noise around fertility lately. Entertainment sites keep rounding up romance-adjacent movies that make “right person, right time” feel effortless, while other headlines remind us that real timelines can be complicated.
At the same time, conversations about “the number 35” keep popping up. The takeaway is more nuanced than a cliff: fertility changes over time, but it doesn’t flip like a switch on a birthday. It depends on multiple factors—egg quality, sperm health, cycle regularity, and overall health.
In that swirl, at-home options like ICI can sound appealing. For LGBTQ+ people, solo parents by choice, and anyone using a donor, home insemination can also feel like a way to build a family on your own terms.
What matters medically (without the scare tactics)
ICI basics: what it is and what it isn’t
Intracervical insemination (ICI) is a method where semen is placed in the vagina near the cervix around ovulation. It’s different from intercourse, but the goal is similar: help sperm reach the cervix during your fertile window.
ICI is also different from IUI (intrauterine insemination). IUI is done in a clinic with washed sperm placed into the uterus. ICI is typically less expensive and less medicalized, but it may be less effective for some people depending on sperm and fertility factors.
The “35” conversation, in plain language
You’ll often hear 35 treated like a hard line. In reality, fertility tends to change gradually, and the pace varies from person to person. Sperm factors matter, too, and they don’t get enough airtime in mainstream chatter.
If the number is stressing you out, you’re not alone. Try to translate the headline into a practical question: “What’s the best next step for my body and my timeline?” That’s where tracking, consistency, and support can help.
A quick note on tech and tracking
Apps can be helpful for pattern-spotting, but they’re not magic. Some people also use smarter predictions or chat-based tools to interpret cycle data. If you’re curious about the broader concept, here’s a neutral explainer on home insemination kit.
Still, your most reliable signals are often simple: ovulation tests, cervical mucus changes, and cycle history.
How to try ICI at home (tools, technique, comfort)
Before you begin: set the scene
Plan for privacy and a low-rush window. Stress doesn’t “ruin” a cycle, but feeling hurried can make the process harder than it needs to be.
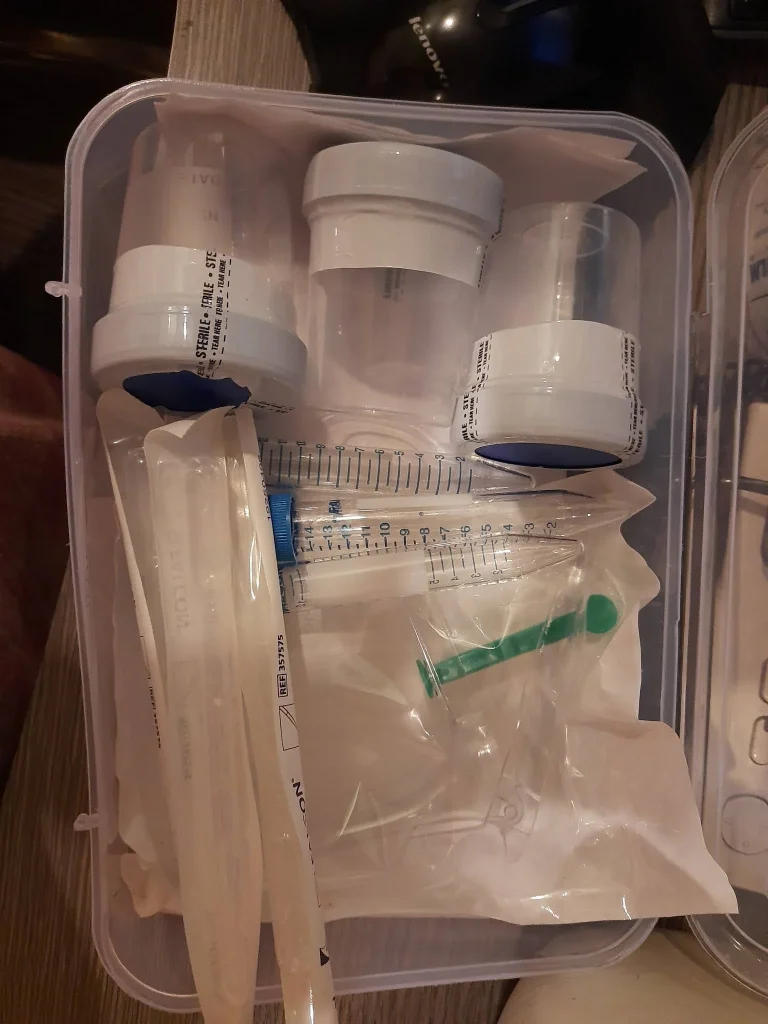
Helpful supplies often include a towel, wipes, a small pillow, and a way to track timing. Many people also prefer a purpose-built option like an at-home insemination kit for ICI rather than improvised tools.
Timing: aim for the fertile window, not perfection
ICI is usually tried close to ovulation. If you use ovulation predictor kits (OPKs), many people aim for the day of a positive test and/or the following day. If you’re tracking cervical mucus, slippery/egg-white-like mucus often signals higher fertility.
If your cycles are irregular, consider tracking for a few cycles before you judge results. Irregularity can make timing tougher, not impossible.
Positioning and insertion: keep it simple
Comfort matters. Many people lie on their back with hips slightly elevated, but you don’t need an extreme angle. Choose a position you can hold without tensing.
Go slowly. The goal is to place semen into the vagina near the cervix, not into the cervix or uterus. If anything feels painful or sharp, pause and reassess.
Aftercare: rest, cleanup, and what “leakage” means
After insemination, resting for 10–20 minutes can feel calming and may reduce immediate leakage. Some fluid coming back out later is common and doesn’t necessarily mean the attempt “didn’t work.”
Use a towel or liner if you want. Then go about your day. Try not to turn the hours afterward into a test of whether you “did everything right.”
When it’s time to get extra support
At-home ICI can be a reasonable first step, but it isn’t the best fit for every situation. Consider talking with a fertility clinician if cycles are very irregular, if you have known conditions that affect ovulation, if there’s a history of pelvic infections, or if sperm parameters are a concern.
Many guidelines suggest seeking evaluation after 12 months of trying if you’re under 35, and after about 6 months if you’re 35 or older. If you’re using donor sperm and carefully timed attempts, you may choose to check in sooner for peace of mind.
Medical disclaimer: This article is for general education and is not medical advice. It can’t diagnose conditions or replace care from a licensed clinician. If you have pain, fever, unusual discharge, or concerns about fertility, contact a healthcare professional.
FAQ: quick answers about ICI at home
Is ICI the same as IUI?
No. ICI places semen in the vagina near the cervix, while IUI places washed sperm into the uterus in a clinic.
Can I use a home insemination kit with frozen donor sperm?
Sometimes, yes. Follow the sperm bank’s instructions closely, and confirm whether your vial type is intended for at-home use.
How long should I rest afterward?
Many people rest for 10–20 minutes for comfort. There isn’t a universally “correct” time.
What’s the biggest timing mistake?
Missing the fertile window by trying too early or too late. OPKs plus cervical mucus tracking can help you narrow it down.
When should I seek help?
If you’ve tried consistently for 6–12 months (depending on age and circumstances), if cycles are unpredictable, or if you suspect a fertility factor, a clinician can help you plan next steps.
Next step: make your next attempt feel less like a storyline
TV pregnancies get written into scripts. Your path gets written one cycle at a time—by your choices, your support system, and what fits your body.
If you want a calmer, more organized way to try ICI at home, start with the basics: timing, comfort, and the right tools.