Five rapid-fire takeaways before you try:
- Timing beats intensity. One well-timed attempt can be more useful than several random ones.
- “35” is a headline number, not a switch. Fertility is influenced by multiple factors for people with eggs and people with sperm.
- At-home ICI is different from IVF. It’s simpler, lower-cost, and less medical—but it’s also less controlled.
- Known-donor legal risk is real. Recent court coverage has people talking about parentage and consent paperwork.
- Track ovulation like it’s your job—briefly. A few minutes a day can protect your energy and improve odds.
What’s trending right now (and why it matters at home)
If you’ve been online lately, fertility conversations are everywhere. Celebrity pregnancy chatter pops up between movie trailers and TV plot twists, and politics keeps showing up in family-building discussions in ways that feel personal. That cultural noise can make it seem like everyone else has a simple path—until you start reading the fine print.
Two themes keep coming up in recent coverage:
- Legal parentage questions around at-home insemination. Headlines about a Florida Supreme Court decision have made many people realize that “donor” and “legal parent” don’t always mean what you think they mean when insemination happens outside a clinic.
- The “fertility cliff at 35” debate. Articles pushing back on the idea of an overnight drop highlight something many LGBTQ+ families already know: bodies are varied, and timelines aren’t one-size-fits-all.
If you want a quick reference point on the legal-parentage coverage people are discussing, see this related update: Florida Supreme Court makes ruling in at-home artificial insemination case.
What matters medically (without the fluff)
ICI (intracervical insemination) is about giving sperm a better starting point than intercourse might provide for some people. It does not bypass the core biology: ovulation has to happen, and sperm has to be present near that window.
The fertile window, in plain language
Pregnancy is most likely when sperm is already waiting in the reproductive tract before ovulation. That’s why the 1–2 days before ovulation often matter as much as ovulation day itself.
Instead of trying to “feel” the right day, use signals you can track:
- Ovulation predictor kits (OPKs): A positive test suggests ovulation may occur soon (often within about a day or two).
- Cervical mucus: Many people notice clearer, stretchy mucus as ovulation approaches.
- Cycle patterns: App estimates can help, but they’re best when paired with OPKs or mucus tracking.
About age and the famous “35”
Age can affect fertility, but it rarely behaves like a trapdoor. Egg quantity and quality, sperm parameters, ovulation regularity, underlying conditions, and plain luck all play roles. If “35” has been living rent-free in your head, you’re not alone—and you’re not behind for wanting a plan that fits your real life.
A quick word on embryo headlines
Every so often, a big story about embryos stored for decades makes the rounds. It can be inspiring, but it can also distort expectations. Storage longevity and success rates depend on many variables, and those stories don’t change what’s most actionable for ICI: timing, preparation, and a clear next step if it doesn’t work quickly.
How to try at home (ICI) with a home insemination kit
At-home ICI can be a practical option for solo parents, queer couples, and anyone using donor sperm. The goal is to keep the process calm, clean, and well-timed.
Step 1: Choose your timing plan (simple is fine)
- If you use OPKs, plan to inseminate around your positive result and/or the following day.
- If you don’t use OPKs, track cervical mucus and aim for the days when it becomes slippery/stretchy.
- If your cycles are irregular, consider adding OPKs to reduce guesswork.
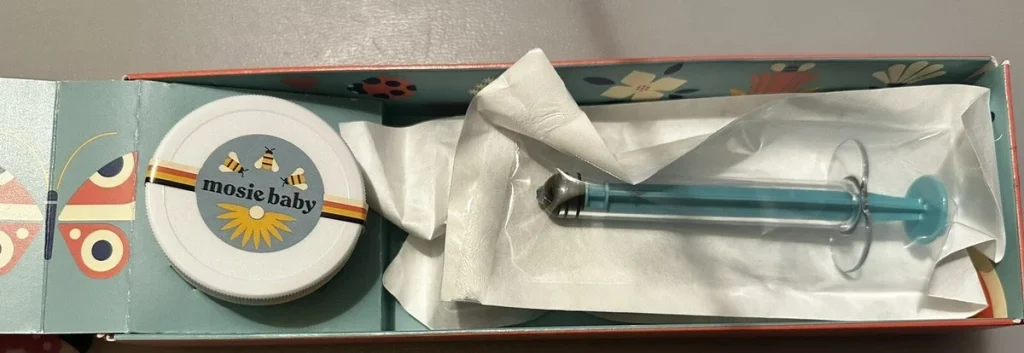
Step 2: Get your supplies ready before the window opens
Scrambling on the day you get a positive OPK is how timing slips. Many people use a at-home insemination kit for ICI so the basics are ready when the window hits.
Step 3: Focus on comfort and consent
Set expectations ahead of time—especially if a partner or known donor is involved. This is a body-centered process, and it should feel emotionally safe. If it doesn’t, pause and adjust the plan.
Step 4: Keep the routine low-drama
Think “calm and repeatable,” not “perfect.” A short setup, clear steps, and a consistent approach reduce stress across cycles. Stress doesn’t cause infertility by itself, but chaos can make it harder to time attempts well.
Step 5: Don’t ignore the legal side (especially with known donors)
If you’re using a known donor, don’t rely on assumptions or handshake agreements. Laws vary, and recent court coverage has pushed these issues into the mainstream for a reason. Consider getting legal guidance about parentage, donor agreements, and second-parent adoption where relevant.
Medical disclaimer: This article is for general education and is not medical or legal advice. It can’t diagnose conditions or replace care from a clinician. If you have pain, unusual bleeding, a known reproductive condition, or questions about medications, talk with a qualified healthcare professional.
When to seek help (and what “help” can look like)
At-home ICI can be a reasonable first step, but it shouldn’t become an endless loop. Consider a check-in with a fertility clinician if:
- You’ve tried 3–6 well-timed cycles without a pregnancy.
- You’re 35+ and you want a faster feedback loop on egg reserve, ovulation, or sperm factors.
- Your cycles are very irregular, very painful, or you suspect endometriosis/PCOS or other conditions.
- You’re using frozen donor sperm and want to discuss whether IUI or IVF could improve efficiency.
“Help” doesn’t always mean IVF tomorrow. It can mean basic labs, an ultrasound, a semen analysis for a partner, or a plan to move from ICI to IUI if timing is solid but results aren’t showing up.
FAQ
Is ICI private and discreet?
It can be. Many people prefer home because it offers control over the environment and less clinical friction.
Can two moms or two parents without sperm do ICI?
Yes. Many LGBTQ+ families use donor sperm and choose ICI at home as a starting option.
Do I need to be on a strict schedule?
No. You need a reliable way to identify ovulation, then aim attempts around that window.
Next step: make your timing easier this cycle
If your goal is to try ICI without turning your life into a spreadsheet, start by picking one tracking method (often OPKs) and preparing your supplies ahead of time.











