- ICI at home can be a real option—especially for LGBTQ+ families, solo parents, and anyone seeking a lower-intervention starting point.
- A home insemination kit helps with consistency, which can reduce stress on “try day.”
- Timing matters more than perfection; a calm plan beats a frantic one.
- Legal and consent conversations are part of the process, not an afterthought—especially with known donors.
- Safety is practical, not scary: clean supplies, appropriate containers, and thoughtful testing choices go a long way.
The big picture: why at-home ICI is having a moment
If you’ve been scrolling lately, it probably feels like pregnancy storylines are everywhere. Entertainment outlets keep pointing out how often an actor’s real-life pregnancy gets written into a show, and that can hit differently when you’re tracking ovulation instead of plot twists. Meanwhile, culture is also leaning hard into escapism—spoofs and nostalgic comedy vibes are back, and romantic watchlists keep circulating. When life feels like a montage, it’s normal to want a family-building option that feels more like your pace.

At-home insemination (often called ICI, intracervical insemination) sits in that “doable” middle ground. It’s less medicalized than clinic-based options, and for many people it feels more intimate and private. It also isn’t a shortcut around biology, and it won’t replace care you may ultimately want. Think of ICI as one tool in a larger fertility toolbox, not a moral stance or a forever decision.
It’s also worth noticing how science headlines can affect expectations. When you see stories about advances in animal reproduction research or lab breakthroughs, it can create a sense that fertility should be “solved” already. Real life is slower. Your body, your relationship(s), and your budget deserve a plan that respects that.
The emotional side: pressure, hope, and communication
When baby news feels like background noise you can’t mute
Celebrity pregnancy gossip and surprise announcements can be oddly activating. Even if you’re genuinely happy for someone else, your brain can still translate it as: “Why not us?” That reaction doesn’t mean you’re bitter. It means you’re invested.
Try giving the feelings a job instead of a megaphone. Name what’s underneath—fear of wasting a cycle, worry about disappointing a partner, grief after prior losses, or anxiety about money. Once it’s named, you can plan around it.
Talk about roles before try day
One of the most underrated parts of at-home ICI is deciding who does what. Who tracks ovulation? Who manages supplies? Who sets the tone if things feel awkward? If you’re using a donor—known or banked—who communicates with them?
These conversations can feel unromantic. They’re also relationship-protective. A simple script helps: “On try day, I need ____,” and “If it doesn’t work this cycle, I’d like us to ____.”
Practical steps: a calm ICI plan you can actually follow
1) Decide what “success” means for this cycle
Yes, the goal is pregnancy. But a cycle can still be a win if you: timed it as planned, kept stress manageable, and learned something about your body. That mindset keeps the process from turning into a referendum on your worth.
2) Get clear on sperm logistics
ICI at home can involve frozen donor sperm from a bank or fresh sperm from a known donor. Frozen sperm adds predictability and screening infrastructure, but it can be expensive and time-sensitive once thawed. Fresh sperm can feel simpler logistically, yet it raises testing, consent, and legal questions that deserve upfront attention.
3) Build a try-day setup that’s simple, not fussy
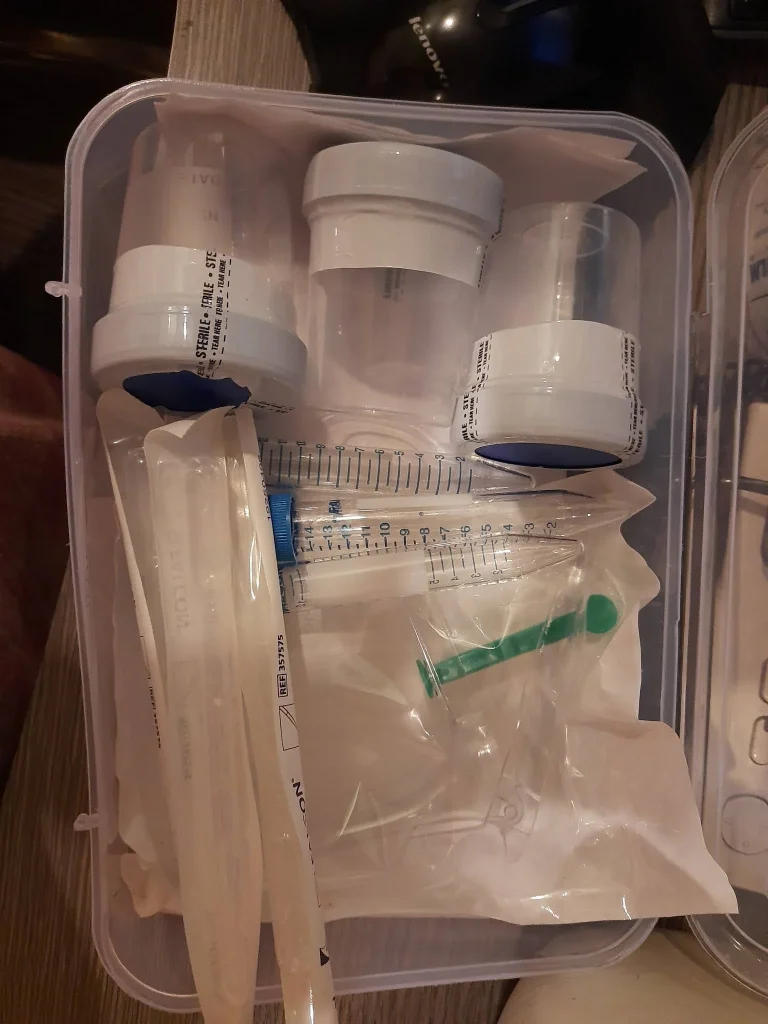
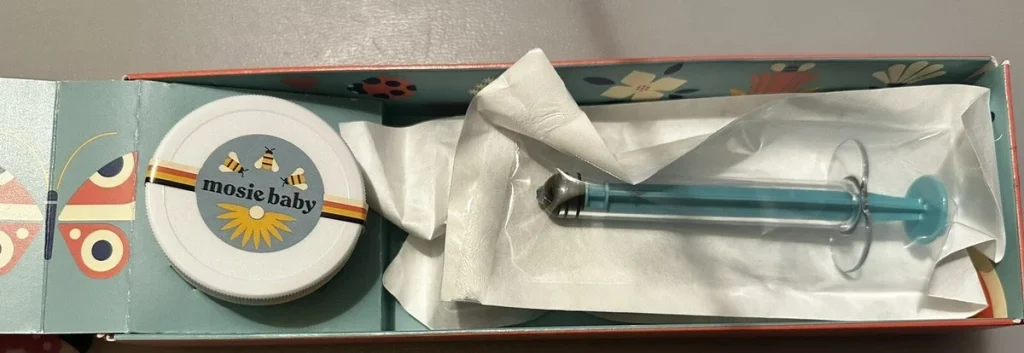
You don’t need a complicated ritual. You need a clean, comfortable space and a plan you can repeat. Many people choose a at home insemination kit to support consistent collection and placement.
Keep your checklist short: supplies, towels, a timer, and anything that helps you feel grounded (music, a show, a snack for afterward). If humor helps, lean into it. A good spoof can be the emotional palate cleanser you didn’t know you needed.
4) Track ovulation with a method you’ll stick with
OPKs are popular because they’re straightforward. Cervical mucus tracking can add useful context. Basal body temperature confirms ovulation after the fact, which can still help you refine timing next cycle.
If you love data, you might be tempted to optimize everything. Remember: fertility tracking isn’t the same as running an algorithm, even if the internet makes it look that way. For a general explainer of the concept behind “smart” tools, see home insemination kit. Use tech as support, not as a judge.
Safety and testing: reduce risk without spiraling
Clean technique and the right materials
Use clean hands, clean surfaces, and materials intended for body-safe use. Avoid improvised tools that aren’t designed for insemination. If anything looks damaged or unclean, don’t use it.
STI testing and donor screening
If you’re working with a known donor, talk about STI testing early and agree on boundaries. Screening doesn’t eliminate risk, but it can reduce it. If you’re not sure what’s appropriate for your situation, a clinician or sexual health clinic can guide you.
Legal reality check (especially with known donors)
Family-building laws vary widely. Recent legal coverage has reminded many people that at-home donor arrangements can lead to unexpected parentage outcomes in some places. If you’re using a known donor, consider consulting a family law attorney who understands LGBTQ+ pathways and assisted reproduction in your region.
FAQ: quick answers before you overthink it
Is ICI painful?
Many people describe it as uncomfortable or strange rather than painful. If you experience significant pain, stop and consider medical advice.
Do we need to orgasm afterward?
Some people try it, others don’t. There isn’t a universal rule. Focus on timing, comfort, and what feels emotionally safe.
How many cycles should we try at home before changing plans?
It depends on age, cycle regularity, sperm type (fresh vs frozen), and health history. If you feel stuck or anxious, getting a consult can provide clarity without committing to IVF.
CTA: make it easier on your relationship (and yourself)
At-home ICI works best when the plan supports your nervous system, not just your calendar. Choose a setup that feels clear, consent-forward, and repeatable—then give yourselves permission to be human about it.
How does at-home insemination (ICI) work?
Medical disclaimer: This article is for general education and is not medical or legal advice. It does not diagnose, treat, or replace care from a qualified clinician. If you have health concerns, fertility conditions, severe pain, or questions about STI testing or medications, please consult a licensed healthcare professional. For legal questions about donors and parentage, consult an attorney in your jurisdiction.