Fertility is everywhere right now. It shows up in celebrity baby speculation, in TV storylines about “the clock,” and in political headlines about reproductive rights.

That noise can make a private decision feel public. You still get to choose a path that fits your body, your relationship(s), and your budget.
At-home insemination (ICI) is a real, practical option—and a home insemination kit can make it safer, calmer, and easier to repeat.
The big picture: why people are talking about home fertility options
Recent reporting has pushed back on the idea that fertility drops off a cliff the moment someone turns 35. Age matters, but it’s not a single-number verdict. Egg supply, ovulation patterns, sperm health, and medical history all play a role.
At the same time, reproductive health policy and court cases keep shifting the landscape. When access feels uncertain, many people look for options they can control at home—especially LGBTQ+ folks, solo parents, and anyone using donor pathways.
And yes, tech is part of the conversation too. People use apps, trackers, and even “smart” predictions to plan tries. If you’ve ever wondered how computers learn patterns in health data, here’s a plain-language starting point: home insemination kit.
The emotional side: what no one posts in the group chat
Trying at home can feel empowering. It can also feel weirdly clinical in your own bedroom, especially if you’re coordinating donors, shipping windows, or long-distance partners.
Give yourselves permission to name what’s hard: pressure, grief, excitement, awkwardness, and hope can all exist in the same week. If you’re a queer couple or solo parent, you may also be carrying the extra labor of explaining your family to systems that weren’t built for you.
A simple plan helps. So does a consent-forward mindset: everyone involved should feel clear, unhurried, and respected—every time.
Practical steps: ICI at home without the chaos
1) Know what ICI is (and isn’t)
ICI (intracervical insemination) places semen in the vagina close to the cervix. It’s different from IUI, which puts washed sperm into the uterus in a clinic.
ICI can be a starting point for people who want a lower-intervention option before moving to clinic care. It’s also common for LGBTQ+ family-building with donor sperm.
2) Time it like a project, not a vibe
You’re aiming for the fertile window around ovulation. Many people use ovulation predictor kits (OPKs), cervical mucus changes, or a fertility tracking app to narrow timing.
If you’re using frozen sperm, timing matters even more because sperm survival time can be shorter than with fresh. If your cycles are irregular, consider extra tracking or a clinician conversation to avoid guessing.
3) Use tools designed for the job
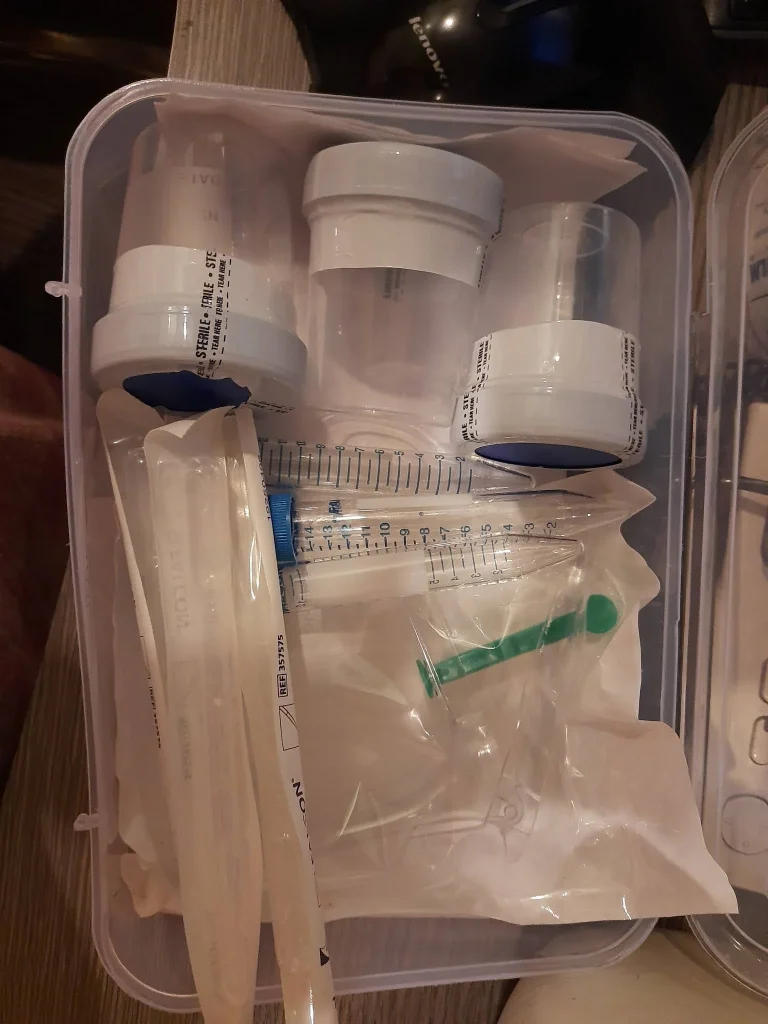
A home insemination kit can reduce fumbling and help you keep things cleaner and more consistent from cycle to cycle. Look for sterile, single-use components and instructions that match your sperm source (fresh vs. frozen).
If you’re comparing options, start here: at home insemination kit for ICI.
4) Create a repeatable “try-day” routine
- Wash hands, clear a clean surface, and keep pets out of the room.
- Confirm donor ID, vial details, and timing notes before you start.
- Move slowly. Rushing increases spills, stress, and mistakes.
- Write down date/time, OPK results, and any symptoms for next-cycle learning.
Safety + screening: reduce infection risk and legal confusion
Choose screening that matches your risk tolerance
If you can, use sperm from a reputable bank with infectious disease screening and clear handling instructions. If you’re using a known donor, talk openly about STI testing, timing of tests, and what happens if results change.
At-home insemination should never involve unsterile tools. Avoid “DIY hacks” that weren’t designed for insemination.
Document decisions like you may need them later
Reproductive rights and parentage rules can vary by state, and they can change. Documentation helps you stay organized and can reduce future disputes—especially with known donors.
- Keep records of donor agreements, receipts, and communications.
- Write down consent from all parties for each cycle attempt.
- Consider legal guidance on parentage in your state before you start.
Know when to bring in a clinician
Home ICI can be a reasonable first step, but it’s not the only step. If you’re not getting clear ovulation signals, if you have known fertility conditions, or if you’ve tried multiple well-timed cycles without success, a fertility clinic can offer testing and options like IUI or IVF.
Medical disclaimer: This article is for general education and does not provide medical advice, diagnosis, or treatment. For personalized guidance—especially around infertility, STI screening, medications, or pregnancy complications—talk with a qualified clinician.
FAQs: quick answers before you try
Is ICI the same as IUI?
No. ICI places semen in the vagina near the cervix. IUI places washed sperm into the uterus and is done in a clinic.
Can a home insemination kit help if I’m over 35?
A kit can help with process and comfort, but age is only one factor. Timing, sperm quality, and underlying health also matter, so consider testing and a clinician consult if you can.
How many times should we inseminate in a cycle?
Many people try once or twice around ovulation. If you’re using frozen donor sperm, talk with your bank or clinician about best timing so you don’t waste vials.
What’s the safest way to handle donor sperm at home?
Use screened donor sperm from a reputable bank when possible, follow storage/thaw directions exactly, and use sterile, single-use supplies. Avoid reusing syringes or improvised tools.
Do we need paperwork if using a known donor?
It’s strongly recommended. A written agreement, consent, and documentation of the method and timing can reduce future legal confusion, though laws vary by state.
CTA: make your next step simple
If you want a home-based approach that’s structured and repeatable, focus on timing, sterile supplies, and documentation. Then build a routine you can actually do again next cycle.