- ICI is simple on paper, but comfort, timing, and setup make the biggest difference.
- “35” is a headline number—fertility doesn’t flip like a switch on a birthday, and partners/donors matter too.
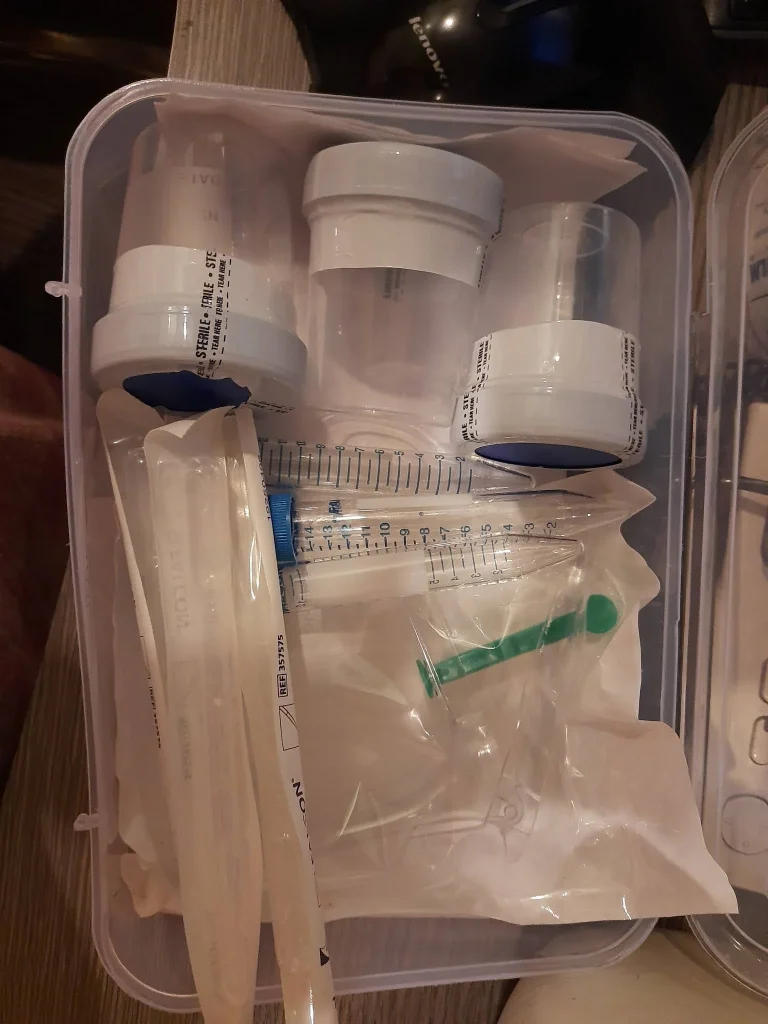
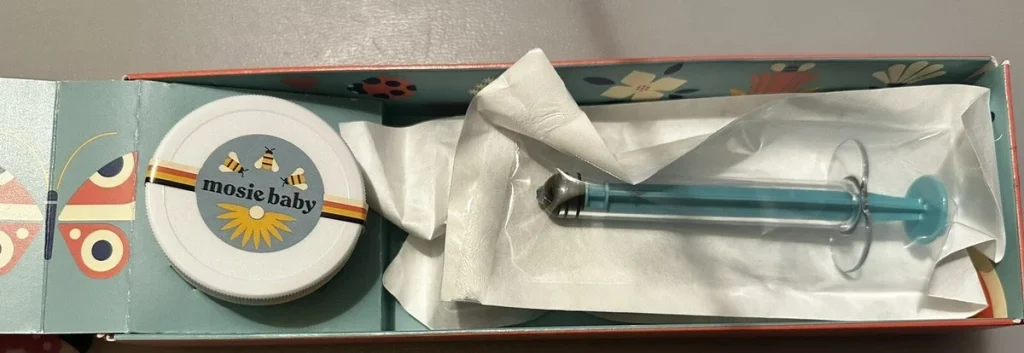
- A home insemination kit helps with control: pace, privacy, positioning, and less mess.
- Try-day emotions are real; plan for nerves the way you’d plan for ovulation tests.
- Safety is not optional: clean hands, correct materials, and a clear stop-sign list.
Big picture: why at-home ICI is trending in the conversation
If it feels like pregnancy storylines are everywhere, you’re not imagining it. Entertainment sites love a “pregnancy written into the show” roundup, and celebrity baby rumors tend to spike whenever a new season drops or a red-carpet look gets dissected. Those cultural moments can be fun, but they also make family-building feel like a public sport.

Meanwhile, real-world fertility coverage has been circling a familiar number: 35. Recent reporting has emphasized that fertility doesn’t suddenly collapse on a single birthday. It’s more nuanced than that, and it includes factors like egg supply, sperm health, cycle regularity, and medical history.
That mix—pop culture noise plus nuanced fertility realities—pushes many people to look for options they can start sooner, at home, and with a clearer budget. For some, ICI is a first step before exploring IUI or IVF. For others, it’s the right fit because of privacy, identity, or donor logistics.
And yes, the broader “tools and tech” wave is here too. People are used to apps, trackers, and algorithmic recommendations in every corner of life, from streaming to shopping. Even a quick home insemination kit shows how much decision-support has entered daily routines. Fertility planning isn’t immune to that mindset, but your body still deserves a human pace.
Emotional considerations: make room for feelings (not just logistics)
At-home insemination can look low-key from the outside. Inside the house, it can feel like a high-stakes performance: get the timing right, do it “correctly,” stay calm, be hopeful, don’t be too hopeful. That pressure is common, especially for LGBTQ+ families who may have already navigated extra steps, extra costs, or extra explaining.
If you’ve experienced loss, ectopic pregnancy, or surgery, fertility-related stress can be intense and surprisingly persistent. Research discussions around fertility stress after procedures highlight how many factors can shape anxiety, from physical recovery to social support. You don’t need to “earn” support—if you’re feeling it, it’s real.
Consider choosing a simple ritual that isn’t about perfection: a playlist, warm socks, a silly show afterward, or a planned walk the next day. It’s not superstition. It’s emotional first aid.
Practical steps: how to use a home insemination kit for ICI (without the drama)
1) Prep your space like you’re hosting Future You
Pick a spot that feels private and calm. Lay out what you’ll need before you start so you’re not rummaging mid-try. Dim lighting helps some people relax, but bright lighting can help others feel more confident. Choose what lowers your stress.
- Clean towel or disposable pad
- Hand soap and clean water
- Timer (phone is fine)
- Optional: pillow(s) for hip support
2) Timing: keep it practical, not mystical
ICI works best when it’s close to ovulation. Many people use ovulation predictor kits (OPKs) and track cervical fluid changes. If your cycles are irregular, you may need more than one method, or more days of testing, to narrow the window.
If headlines about a “fertility cliff” have you spiraling, zoom out. Age is one factor, not a verdict. If you’re unsure about your cycle patterns or you’ve been trying for a while, a clinician can help you decide what to test next.
3) Handling and comfort: slow is smooth
Follow any instructions that come with your sperm source and your supplies. If you’re working with donor sperm, storage and thaw guidance matters. Rushing creates spills, stress, and sore muscles.
Use a steady hand and a gentle approach. ICI is not the same as pushing through the cervix. If something hurts, stop and reassess rather than forcing it.
4) Positioning: choose “easy to hold,” not “internet perfect”
People try all kinds of positions. The best one is the one you can maintain comfortably. Many choose to lie on their back with hips slightly elevated, but side-lying can be just as manageable, especially if you’re tense.
After insemination, resting for a short time can reduce immediate leakage and help you feel less rushed. Ten to twenty minutes is a common comfort-based choice.
5) Cleanup: plan for gravity, not failure
Some fluid leakage is normal afterward. It doesn’t mean the attempt “didn’t work.” A towel, pad, or period underwear can make the rest of your day feel more normal. This is one of those small details that can protect your mood.
Safety and testing: what to double-check before you try
Use the right tools
A purpose-built at-home insemination kit for ICI is designed for comfort and control. Avoid improvised items that could splinter, break, or irritate sensitive tissue.
Hygiene basics that matter
- Wash hands thoroughly before and after.
- Use clean, unopened components.
- Don’t share devices between people unless they’re designed for safe reuse and properly sanitized.
Know your “stop signs”
Skip ICI and contact a clinician urgently if you have severe pelvic pain, fever, fainting, heavy bleeding, or symptoms that worry you—especially with a history of ectopic pregnancy or recent pelvic surgery. At-home insemination should never require you to push through sharp pain.
When to consider clinic support
If you’ve tried multiple well-timed cycles without success, or if you suspect ovulation issues, fibroids, endometriosis, or sperm-related factors, talk to a fertility clinician. ICI can be a meaningful step, and it can also be part of a bigger plan that includes labs, imaging, or options like IUI/IVF.
FAQ: quick answers people ask before they buy a kit
See the FAQs above for the most common questions about ICI vs. IUI/IVF, donor sperm, orgasm myths, how long to rest, and safety mistakes to avoid.
CTA: make your try-day plan feel doable
If you want a calmer, more organized way to approach ICI, start with a plan you can repeat. The goal is not to turn your bedroom into a clinic. It’s to give yourself a clear routine that supports timing, comfort, and cleanup.
How does at-home insemination (ICI) work?
Medical disclaimer: This article is for general education and is not medical advice. It does not diagnose or treat any condition. If you have pain, bleeding, fever, a history of ectopic pregnancy, or concerns about fertility, please consult a qualified healthcare professional.