Myth: “If you’re not pregnant by 35, you’ve missed your chance.”
Reality: Age matters, but fertility doesn’t fall off a cliff on one birthday. It shifts over time and depends on many factors—cycle patterns, egg and sperm health, timing, and overall health.

That’s partly why at-home fertility options keep showing up in everyday conversation. When pop culture weaves real pregnancies into TV storylines, it can make family-building look effortless and perfectly timed. In real life, it’s often more like a season-long arc: hope, plot twists, and lots of honest conversations.
The big picture: where ICI at home fits (and where it doesn’t)
Intracervical insemination (ICI) is a way to place sperm near the cervix around the fertile window. For some people, it’s a first step before clinic care. For others, it’s a meaningful choice because it feels private, familiar, and more accessible.
ICI is not IVF, and it’s not a guarantee. Still, a home insemination kit can help you do the basics more cleanly and comfortably than improvising. Think of it as reducing friction in the process, not “hacking” biology.
And yes—timing talk is everywhere right now. Between “fertility cliff” debates and the popularity of ovulation calculators and ovulation tests, it’s clear people want simple answers. The best approach is usually steady and practical, not panicked.
The emotional side: pressure, pacing, and protecting your relationship
Try cycles can turn into a monthly referendum on your body, your partnership, and your future. That pressure can sneak in even when you’re excited. It can also hit harder for LGBTQ+ families navigating donor decisions, disclosure questions, and extra logistics.
Two check-ins that keep try days from taking over
Name the storyline you’re living in. Is this month “we’re hopeful,” “we’re exhausted,” or “we need a reset”? Saying it out loud lowers the temperature.
Decide what counts as a win. A win might be “we communicated,” “we followed our plan,” or “we stayed kind.” Pregnancy is the goal, but it can’t be the only measure of success.
Practical steps: a grounded ICI plan for home
Here’s a simple way to plan without turning your kitchen into a lab.
1) Pick your tools (keep it simple)
Many people combine a calendar-based ovulation estimate with ovulation predictor kits (OPKs). Some also track cervical mucus or basal body temperature. You don’t need every method at once; too many inputs can create more stress than clarity.
2) Map your “likely window,” then narrow it
Start broad (your likely fertile window), then narrow based on OPKs. If your cycle varies, give yourselves extra emotional slack. Irregular cycles are common, and they can make timing feel personal when it’s not.
3) Set the scene like a calm routine, not a performance
Try day tends to go better when you plan for comfort: privacy, a clean surface, and a few minutes without interruptions. If you’re using donor sperm, confirm thaw timing and handling instructions ahead of time so you’re not reading fine print while stressed.
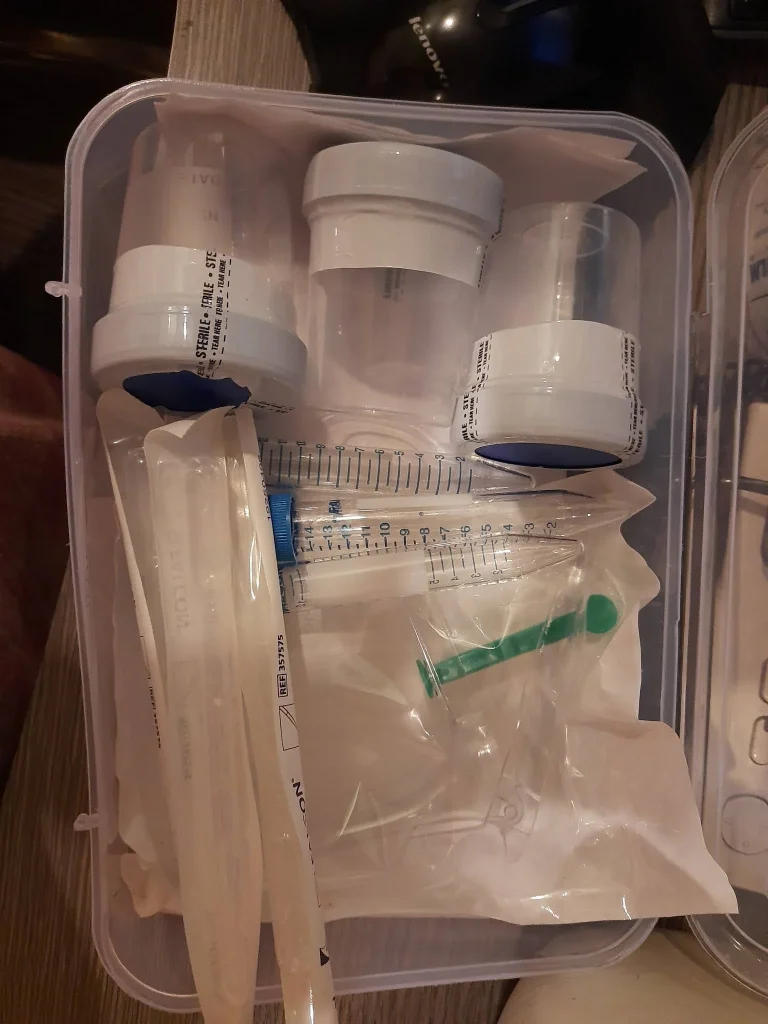
4) Use a purpose-built kit rather than improvised tools
People sometimes reach for whatever is around, especially when they feel urgency. That’s where frustration and mess can spike. A purpose-built option like an at-home insemination kit is designed for the job, which can make the process feel more controlled and less clinical.
Safety and testing: what to prioritize (and what to skip)
At-home insemination should be clean and gentle. Focus on reducing infection risk and avoiding anything that could irritate tissue.
Hygiene basics that matter
- Use sterile, single-use components; don’t reuse syringes or containers.
- Wash hands and prep a clean surface.
- Avoid unapproved lubricants; some can be sperm-unfriendly.
Testing and timing tools: helpful, not moral
OPKs and ovulation calculators are popular because they offer a sense of control. That’s valid. Just remember they’re estimates, not verdicts. If you find yourself spiraling over numbers, it may help to simplify your tracking for a cycle.
A note on “smart” fertility tools
You may see apps that claim they can predict everything. Some use pattern recognition and advanced analytics, sometimes marketed with terms like home insemination kit. These tools can be useful for organizing data, but they can’t replace medical evaluation or guarantee timing accuracy for every body.
Medical disclaimer: This article is for general education and is not medical advice. It does not diagnose or treat any condition. If you have pain, abnormal bleeding, a history of infertility, or concerns about donor sperm handling, talk with a qualified clinician.
FAQ: quick answers people ask before they try ICI at home
Is ICI painful?
It’s usually described as mild pressure or discomfort, not severe pain. Stop if you feel sharp pain and consider medical guidance.
How many cycles should we try before changing the plan?
It depends on age, cycle regularity, and medical history. If you feel stuck, a clinician can help you decide whether to adjust timing, run basic labs, or discuss IUI/IVF.
Can stress “ruin” a cycle?
Stress can affect sleep, libido, and routine, which can indirectly affect timing. It’s not a personal failure. A simpler plan and better support can help.
CTA: make a plan you can live with
If you’re considering ICI, aim for a process that protects your relationship and your mental health. The goal is not to do everything—it’s to do the right few things consistently.