Is a home insemination kit actually worth trying before IVF?

How do you time ICI at home so you don’t waste a cycle?
What’s the real risk—medical, emotional, and legal—when you do this outside a clinic?
Yes, a home insemination kit can be a practical first step for some people, especially when you want a lower-cost, lower-intervention option than IVF. Timing and preparation matter more than fancy gear. And right now, the cultural conversation is louder than usual—between TV storylines that touch pregnancy loss, celebrity pregnancy buzz, and court decisions that remind everyone that “at-home” doesn’t mean “no rules.”
The big picture: why ICI at home is having a moment
At-home insemination (ICI, intracervical insemination) sits in a sweet spot: more hands-on than “just see what happens,” but far less expensive and clinical than IVF. For LGBTQ+ families, solo parents by choice, and couples dealing with timing, travel, or privacy concerns, ICI at home can feel like a way to keep momentum without immediately stepping into a full fertility workup.
At the same time, headlines have made one thing clear: reproductive health is not just personal—it’s political and legal. Court cases and ongoing litigation discussions keep shifting what people assume is “safe” or “standard.” If you’re considering a known donor, the legal side deserves the same attention as ovulation timing.
If you want a quick reference point for the legal conversation making news, see this: Florida Supreme Court makes ruling in at-home artificial insemination case.
Emotional considerations: hope, pressure, and the stories we absorb
Pop culture doesn’t create your feelings, but it can turn the volume up. When a big show debates whether a pregnancy-loss storyline is “too much,” it reflects a real tension: many people want honesty about loss, yet they also crave escapism. If you’re trying at home, that push-pull can show up as, “I should be chill about this,” right next to, “I can’t stop thinking about it.”
Give your plan emotional guardrails. Decide in advance how you’ll handle social media spirals, celebrity pregnancy chatter, and well-meaning friends who treat conception like a simple plot twist. Also talk through what “support” looks like on insemination day—privacy, rituals, humor, silence, or a backup person you can text.
Important note: Pregnancy loss can be common and also deeply painful. If you’ve experienced loss, consider extra support (a counselor, a support group, or a trusted clinician) while you try again.
Practical steps: a no-waste-cycle ICI plan
This is the part most people wish they’d simplified sooner. A solid at-home ICI attempt is mostly about preparation and timing—not improvising at the last minute.
1) Choose your sperm pathway (and align it with your budget)
Two common routes are banked donor sperm (often frozen) or a known donor. Banked sperm can cost more per vial, but it often comes with standardized screening. Known donor arrangements can lower some costs, yet they can add legal and logistical complexity.
2) Track ovulation like it’s your job—for one week
You don’t need months of charts to start. You need a focused plan for the fertile window:
- Use ovulation predictor kits (OPKs) to detect an LH surge.
- Notice cervical mucus changes (often becomes clearer and more stretchy near ovulation).
- Use a calendar or app to estimate your likely window, then confirm with OPKs.
If your cycles are irregular, you may need more OPKs on hand. That’s often cheaper than “guessing” and losing a month.
3) Keep the setup simple (and cervix-focused)
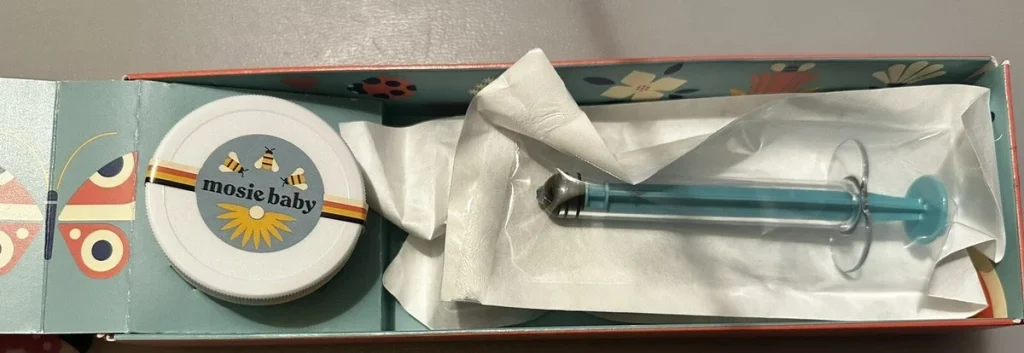
ICI places sperm near the cervix. You’re not trying to enter the uterus at home. A purpose-built kit can help with comfort, control, and minimizing mess. If you’re shopping, look for a kit designed for ICI and follow the included instructions carefully.
If you’re exploring options, this at-home insemination kit for ICI search is a useful starting point for comparing what’s included.
4) Plan for two attempts (if your sperm type allows it)
Some people try once; others aim for two well-timed attempts around the surge/ovulation window. What’s feasible depends on sperm availability, sperm type, and cost per attempt. If each try is expensive, prioritize the single best-timed attempt rather than spreading resources thin.
Safety and testing: reduce risk without overcomplicating it
At-home does not mean “do whatever.” It means you take responsibility for basics that clinics usually manage.
Use only body-safe, clean materials
Use sterile or single-use components when possible, and avoid household items not intended for this purpose. Stop if you feel sharp pain, dizziness, fever, or heavy bleeding, and seek medical care.
Be cautious with fresh sperm and unknown screening
Frozen sperm from regulated banks is typically screened under established protocols. With known donors and fresh samples, risk management can involve STI testing, clear storage/handling practices, and honest conversations about exposure windows. A clinician can advise on what testing makes sense for your situation.
Don’t skip the legal conversation (especially with known donors)
Recent reporting has highlighted that at-home arrangements can create unexpected legal outcomes. Depending on where you live, a donor could be treated as a legal parent if steps aren’t handled correctly. Consider a family-law attorney familiar with assisted reproduction in your jurisdiction before insemination.
FAQ: quick answers before you buy anything
Is ICI painful?
Many people describe it as uncomfortable or neutral, similar to inserting a tampon. Pain isn’t the goal. If you experience significant pain, stop and consider medical guidance.
Do I need to orgasm for ICI to work?
No. Some people choose to because it can help them relax, but it’s not a requirement.
What if I have PCOS, endometriosis, or low sperm count concerns?
Those factors can affect outcomes and may change which options make sense. A clinician can help you decide whether home ICI is reasonable or if testing/treatment would save time and money.
Next step: make your plan for this cycle
If you’re choosing ICI at home, treat it like a small project: supplies ready, timing tools stocked, and a clear decision on donor pathway. That’s how you protect your budget and your energy.
How does at-home insemination (ICI) work?
Medical disclaimer: This article is for general education and does not provide medical advice, diagnosis, or treatment. Fertility and pregnancy involve individual risks. If you have health conditions, a history of pregnancy loss, signs of infection, severe pain, or questions about STI testing or medications, consult a licensed clinician.